For people with epilepsy, a seizure can occur without warning, causing sudden loss of consciousness and a dangerous convulsion. Medications can prevent seizures for some patients, but more than a third of patients continue to have attacks despite using appropriate seizure medications. Seizures occur when there is an imbalance in the pattern of electrical impulses that excite and inhibit nerve cells in the brain, causing brain networks to be unstable. Understanding how brain networks differ between people who have epilepsy and those who don’t could provide new strategies for helping the three million people In the U.S. who suffer from this challenging disorder.
Researchers in the UConn Department of Neurology have begun to investigate how brain networks differ between people who have epilepsy and those who don’t. Principal investigator Dr. John Greenfield, Chair of the Department of Neurology at UConn Health, working with Stefan Sumsky, a postdoctoral biomedical engineer, devised a new method for examining brain networks in patients based on their EEG waves. This new approach uses mathematical models to determine the structure of the brain network and how it changes during a seizure. According to Greenfield, “Studying brain networks could provide new insights into how seizures occur and suggest new treatments.”
Their initial studies were based on recordings from patients who had electrodes implanted in their brains to determine the sources of their seizures for epilepsy surgery. However, implanted electrodes are only used for the most challenging cases of epilepsy. To apply this information more broadly, the method needed to be extended to regular EEGs performed with electrodes on the scalp, with enough electrodes to map out the seizure network.
 UConn has a High-Density EEG machine that uses a large number of electrodes on the scalp, but it has not been used in recent years since the COVID pandemic shut down early research projects. To help get the system up and going again, Greenfield recruited second-year UConn School of Medicine student Chelsea Rutagengwa. Rutagengwa received a prestigious summer research scholarship from the American Academy of Neurology to investigate whether high-density EEG could show the differences in brain networks between people with epilepsy and those without.
UConn has a High-Density EEG machine that uses a large number of electrodes on the scalp, but it has not been used in recent years since the COVID pandemic shut down early research projects. To help get the system up and going again, Greenfield recruited second-year UConn School of Medicine student Chelsea Rutagengwa. Rutagengwa received a prestigious summer research scholarship from the American Academy of Neurology to investigate whether high-density EEG could show the differences in brain networks between people with epilepsy and those without.
Rutagengwa knew during her junior year of high school in New Hampshire that she was interested in the brain and neuroscience. She then attended Northeastern University in Boston as a behavioral neuroscience major. Following graduation, she took a few GAP years to determine where she wanted to take her career in this field. She worked as a research technologist in the sensorineural hearing lab at Massachusetts Eye and Ear Infirmary in Boston and then volunteered at a hospital to gain experience working with patients. While she enjoys research, she also likes having a relationship with patients and solving problems on a case-by-case basis. Rutagengwa chose UConn School of Medicine because she liked the overall approach to clinical, research and community involvement that the school embodied.
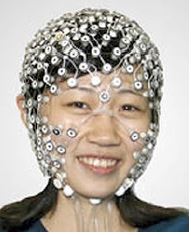
Rutagengwa will use UConn’s High-Density Electroencephalography (HD-EEG), a non-invasive technology that records brain waves using a stretchy net of electrodes that fits over the head like a swim cap. The large number of electrodes can detect atypical brain activity with great accuracy. A typical electroencephalogram (EEG) has 20 electrodes as compared to the HD-EEG which has 256 electrodes, aligned using multiple cameras in a geodesic dome.
Subjects who pass the screening criteria and participate in the study will have the geodesic electrode nets fitted to their head. Their brain waves will be recorded for one to two hours, during which they will be asked to perform some simple tasks, like hyperventilating for a few minutes, looking at flashing lights, and trying to get drowsy and sleep for as long as possible.
After the recording, participants will sit under a geodesic dome equipped with 11 cameras that will take a photo of the net around their heads. With this image, the computer system will be able to sync each electrode’s profile with its unique position on the patient’s head. This is the final step before they complete the study, and no additional appointments are required.
“The goal of the study data is to understand how the connectivity of brain waves differs among those with epilepsy leading to better technology, diagnosis, and treatment of the disease,” says Rutagengwa.
Rutagengwa may use her research experience to establish a career in neurology. “We are always looking to recruit talented clinician-scientists like Chelsea into our neurology residency program,” says Greenfield. “We think she has enormous potential as a future neurologist.”
For further information: please contact Chelsea Rutagengwa or Laxman Kadel at the Clinical Neurophysiology Suite, Department of Neurology at 860-679-5194
This study was approved by the UConn Health Institutional Review Board, IRB# 23-208S-2



