Annamarie Shand says when she learned she was HIV-positive, she knew her life was over.
What she didn’t know at the time was how wrong she would turn out to be.
It was 1992, a time when such a diagnosis was largely considered a death sentence. She contemplated taking her own life. Instead she called an 800 number for guidance, and a counselor referred her to UConn Health.

Shand was under the care of Dr. John Shanley for 15 years, and became Dr. Kevin Dieckhaus’ patient when Shanley retired.
“I was given the ultimate care by my medical team, which included nurses and medical case managers from the very beginning,” Shand says. “I didn’t think I could survive, but my care at UConn is the reason I am still here today living and breathing.”
Yesterday, the Unionville resident celebrated her 58th birthday.
“There’s no way I still would be living with HIV if I hadn’t been here,” Shand says.
André McGuire, 65, has lived with HIV for three decades, and for the last 10 years he’s been a patient of Dr. Lisa Chirch.
“She’s been great,” McGuire says. “She stays on top of new things. I don’t have to go in there and worry about whether or not she’s heard about some of the newer stuff, because she has.”
McGuire says his treatment over the years has kept his HIV largely undetectable.
The longevity of both patients is a testament to their treatment adherence, the term used to describe those who stay current with the recommended medications.
But often, those living with HIV are dealing with more than managing their viral load, and another factor in their success is the support services available through the Ryan White HIV/AIDS Program, which has been in place at UConn Health for more than 20 years.
“The Ryan White staff provides a valuable service in medical navigation and care coordination for HIV patients,” says Dieckhaus, chief of UConn Health’s Division of Infectious Diseases. “As an extension of traditional medical services, Ryan White care coordinators provides patient-centered care that emphasizes linkage to medical care and adherence to medications. However, importantly, the team also addresses the myriad of social, economic, mental health, and other issues that can potentially impact medical outcomes in those with HIV infection.”
Named for an Indiana boy who was 13 when he was diagnosed with AIDS after a 1984 blood transfusion, Ryan White is a federal grant-funded program for patients to help remove barriers to managing their disease.
Patients who have established care with a UConn Health infectious diseases provider and who meet certain income qualifications are eligible for UConn Health’s Ryan White program. Clinical staff help with treatment adherence and preventive care, and medical case managers help them with resources to meet their other needs, such as recommended medical appointments, transportation, utilities, food, prescriptions, housing, and clothing.
Amy Clark is the assistant nurse manager who oversees UConn Health’s Ryan White program, which exists within the infectious diseases practice. She says the face of the Ryan White program is nurse Dezrene Atkinson.
“If you’re new to our clinic or newly diagnosed with HIV, Dezrene is the first person who’s going to come out and see you and talk about barriers,” Clark says. “She administers vaccines, assists with scheduling medical and dental appointments, and will coordinate clinic services.”
Eileen is my crutch… She goes above and beyond for us. And when you see people do that you tend to try to do your part as far as following directions, keeping up with your medical care. — Annamarie Shand
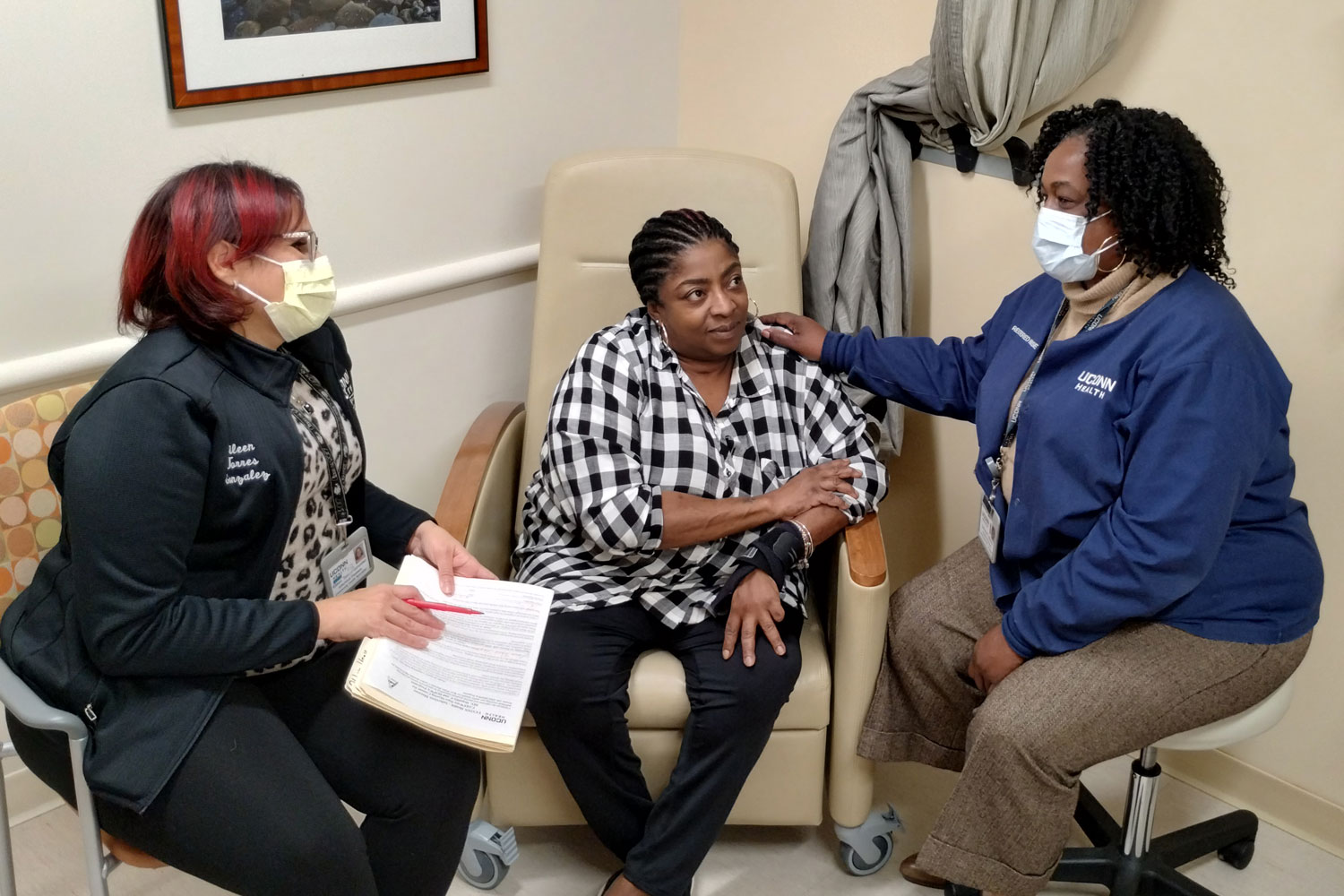
Joining Atkinson and Clark on the team are treatment adherence nurse Jeanne Urso, community health specialist Eileen Torres Gonzalez, and community health worker Blaise Gilchrist.
“Our ultimate goal is for patients to stay in care and feel welcome when they come to the clinic,” says Clark, who also is a treatment adherence nurse. “Anytime a Ryan White patient comes for an office visit we make ourselves available, whether it’s myself as treatment adherence nurse or a medical case manager, we want to make sure that health care services and barriers are being addressed.”
Clark uses a recent interaction to illustrate how patients become clients: An infectious diseases physician referred the patient, noting some of her challenges, and Gilchrist met with her.
“He described what our services are, and she identified that she does need help with transportation, that she does need help filling out energy assistance paperwork, because she recently lost her house, and does not have winter clothing, so we can set her up with that,” Clark says. “She’s taking her medicine as prescribed, so she did not need my service for treatment adherence.”
Others have need for both case management and treatment adherence, and are paired up with Gilchrist or Torres Gonzalez to be their case manager.
“At a minimum, our case managers connect with our patients monthly,” Clark says. “Some of our clients need more support and will reach out daily or weekly. Our case managers are a solid source of support and have become like family. They are often open to sharing their struggles with family, employment, mental health, or substance abuse.”
Torres Gonzalez has been working with Shand as her case manager for about 15 years. She credits that relationship for keeping her healthy, and believes the medical case management is the most important aspect of the Ryan White program.
“All of my services that I get for my health comes through my medical case management; they don’t miss a thing,” Shand says. “Eileen is my crutch. Eileen is that push you need when you feel like your buttons don’t work anymore, when you don’t have the energy to get up and do it anymore. She goes above and beyond for us. And when you see people do that you tend to try to do your part as far as following directions, keeping up with your medical care.”
Torres Gonzalez also has served as McGuire’s case manager.
“She’s able to find everything,” McGuire says. “If I needed help with something, I just told her what it was and she’d figure it out. And then I appreciated that because I already had enough things that I had to deal with in terms of trying to make sure I had a place to stay, trying to make sure that I had income, trying to make sure that I had food. And they even helped with transportation a great deal. Having somebody there who had an understanding of the program and was willing to do some of the legwork to get some of the needed services was a big relief.”
That’s one of the things that I appreciate about being there at UConn, because that was their goal. It wasn’t to keep you there forever, but to prepare you to move on.
— André McGuire
“I want to make sure that they know that I am here to help them, and my best interest is that they remain healthy,” Torres Gonzalez says. “Where I’m coming from, I have no problem telling them, ‘You haven’t picked up your medication in a week, it’s been there at the pharmacy. Why haven’t you picked it up? You missed two appointments in a row. I am here to help you, and I want you to be healthy, but if you don’t comply with your end of the bargain, then how am I going to help you?'”
Shand acknowledges the importance of this, and says it’s another reason for her survival.
“Not everybody is honest with their life, not everyone is as open as I am,” Shand says. “So when you’re not open with your doctors, or your case managers, or whatever support you’re getting, your life is like a circle, you’re just going around in that circle and it never stops. So not only is Eileen dealing with someone like me, I’m open with HIV and I listen and I’m happy with my services, but then you have some people who may take their income and they’re doing drugs, but they’re not going to tell her that.”
Even so, Torres Gonzalez says she can often tell when clients are struggling with drugs or alcohol even when they don’t admit it. What she struggles more with is helping clients get past the stigma of HIV that often persists.
“That is the biggest challenge,” Torres Gonzalez says, “Clients are not wanting to come to their medical appointments because there’s a big sign there that says ‘Infectious Diseases.’”
Clark notes that there is no distinction in the waiting area that makes patients identifiable by their condition.
McGuire, who lives in Waterbury, is the founder and pastor of ALM’s Ministries International, a Hartford nonprofit with a mission of building struggling neighborhoods through education, support, resources, and the Christian faith. With steady employment, transportation, and his own home, he effectively has graduated from UConn Health’s Ryan White program, in that he no longer requires a regular case manager.
“They’ve done quite a bit to help me move along to where I need to be,” McGuire says. “There are other people who will come behind us who are going to need some help. I know not everyone is capable, but for those who are, we need to work with them to a point where they can become independent. And that’s one of the things that I appreciate about being there at UConn, because that was their goal. It wasn’t to keep you there forever, but to prepare you to move on.”
And in the meantime, it’s about removing obstacles.
“UConn is my safety net,” Shand says. “I don’t have to worry about it, if something happens to my medical, I can still get my medication, they’ll cover certain doctor visits. If I have, God forbid, a problem with homelessness or anything, they have so many different programs to use here.”
I can assure anyone needing HIV or medical care that at UConn, U CAN survive! — Annamarie Shand
The medication regimen has become less complex, making treatment adherence less of a challenge than it was in the 1990s. UConn Health Ryan White clients range in age from the 20s to the 70s; their needs range too.
“We have patients who will come to the clinic for an appointment with another specialty and will want to see their case manager and say, ‘Do you have a minute,’” Clark says. “Transportation is often difficult. Many of our patients take the bus or will have other arranged transportation, so they will stop by or schedule a visit with their case manager after a scheduled clinic visit with their providers for assistance with scheduling appointments, filling out paperwork, or job applications.”
Case managers will visit people in their homes, sometimes to drop off bus passes, other times to get paperwork signed.
“One of our philosophies is, ‘Meet you where you are,’” Clark says.
In 1996, Shand had a daughter, born HIV-negative, who remains so to this day at age 27. She credits a drug she took as a participant in a clinical trial at UConn for making that possible. She makes a point of sharing this because she wants to “inform any woman who is pregnant and afraid to get care.”
And she has a message for others living with HIV:
“I can assure anyone needing HIV or medical care that at UConn, U CAN survive,” Shand says. “Thank you, UConn Health, for giving me the care and tools to survive!”
Patients who have established care with a UConn Health infectious diseases provider and who meet certain income qualifications are eligible for UConn Health’s Ryan White program.
Learn more about the Ryan White HIV/AIDS program, which is overseen by the federal Health Resources and Services Administration.
Learn more about UConn Health’s Division of Infectious Diseases.
World AIDS Day is Dec. 1.



