For someone who turned 50 and then ran 13 half-marathons in a 12-month period, simply finishing a 5-mile race may not seem like much of an accomplishment.
But Sherri Beck has a different outlook. A 2021 bout with COVID-19 that started off seemingly innocuous touched off more than two years of health problems that made crossing the finish line a major accomplishment.
“I had a very mild case to start,” Beck says of her COVID diagnosis that March. “I was following all the restrictions. Back then, it was, don’t even leave your house. It was really, really strict, and I followed it to a T because I didn’t want to get anybody else sick. I did exactly what I was supposed to do.”
Beck was 51 at the time, recently had completed a full marathon, and was planning to run in the Hartford Marathon that fall.
“I do love running,” she says. “I’m not fast, but it’s my love. I love being outside, with my running friends. It’s just something I enjoy doing. I felt like I was pretty darn healthy. Especially just before I got COVID, I felt strong.”

She recalls having energy to burn and spending much of her two weeks of isolation with her hula hoop and her elliptical machine to tire herself out so she could sleep at night.
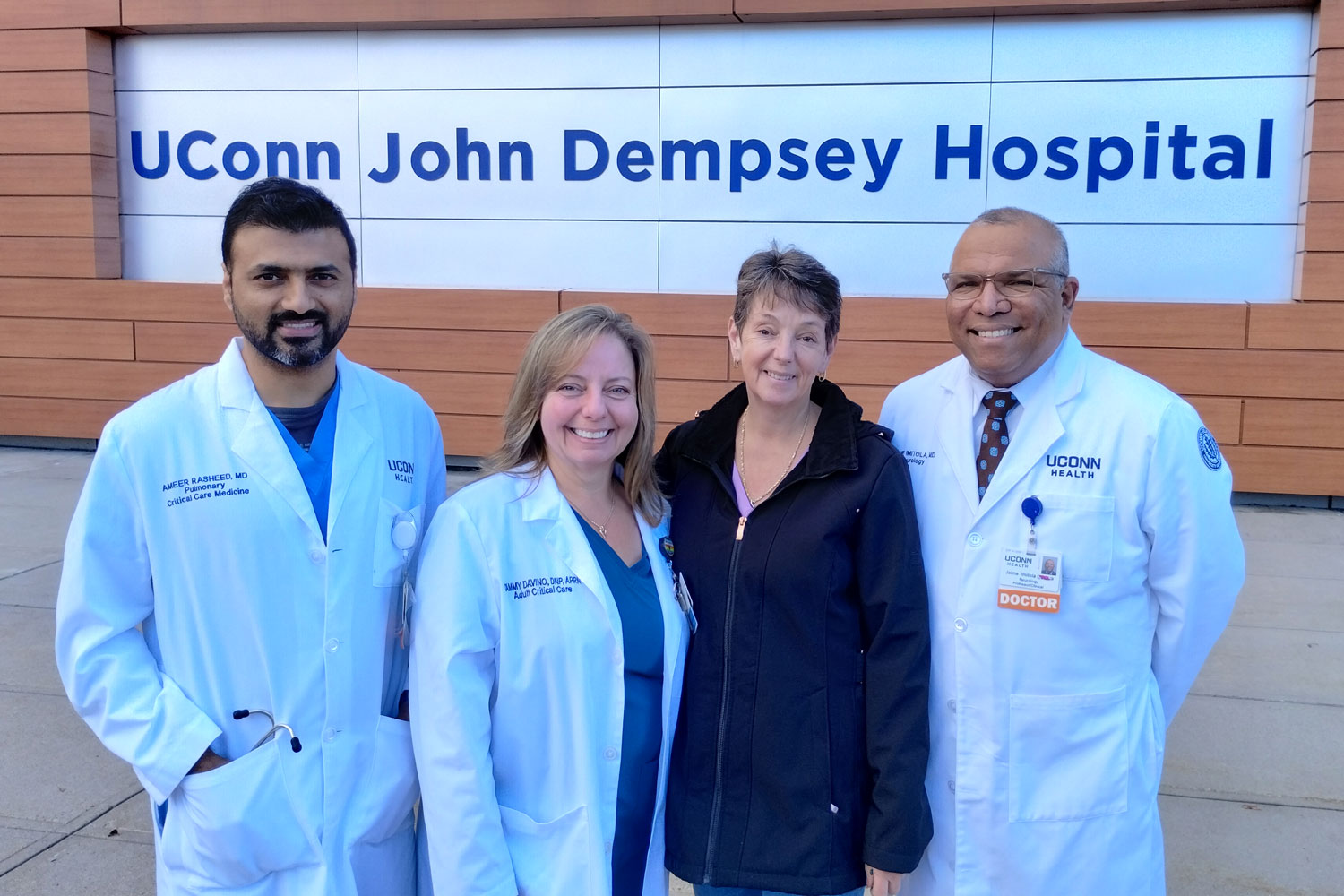
Her sister, Tammy Davino, a nurse practitioner in the UConn John Dempsey Hospital intensive care unit, would check in with her daily.
“Early COVID, we were concerned that there was going to be a procoagulopathic thing — people would develop clots associated with it,” Davino says. “So we never really knew. In the early phases, when she would have some symptoms and I would say, let’s get some care for this.”
Davino recalls the need to stay grounded upon learning about her sister’s diagnosis, against the backdrop of the previous year seeing some of the worst cases of COVID-19 on her own hospital floor.
“You saw variability in how COVID affected people, so you have to keep it all in perspective and you can’t jump to conclusions,” Davino says. “You have to check in and say, ‘How are you feeling and what are your symptoms and are you OK at home?’ And that type of thing. And Sherri’s like, ‘Oh, my God, I’m fine. I don’t have any trouble breathing. I’m just a little tired,’ whatever it was. So with respect to the acute COVID, like when we saw patients in the ICU, it wasn’t as concerning”
Then, about a month after she thought she had gotten over COVID-19, Beck started having different types of symptoms.
“Every day I would send Tammy a text and I would say, ‘bad headache,’ or ‘fever,’ or ‘exhausted by 9 o’clock in the morning,’ whatever the symptoms were,” Beck says. “I had neuropathy in my legs, I had all different types of things that were going on.”
It was becoming clear her short-term memory was failing and she was developing neurological problems. The texts to Davino would serve as a log of her health problems.
The care at UConn Health was phenomenal, and so I kept coming here with all the different scenarios that happened. — Sherri Beck
A certain amount of time would have to pass before Beck would become eligible to be seen by Dr. Ameer Rasheed in the long COVID clinic. During that wait she found herself in the emergency department with chest pain, but her heart was determined to be fine and she went home.
Rasheed describes Beck as having unexplained respiratory symptoms when he first met her, August 2021.
“I performed a comprehensive evaluation and pulmonary testing for her on respiratory symptoms for several months,” Rasheed says. “She was having hard time going back to exercise. I taught her respiratory exercises and made sure her lungs were strong enough to handle personalized exercise program to alleviate her breathing difficulties.”
More and New Problems
The chest pains would come and go, along with stabbing abdominal pain, and problems with her left eye.
“All these little things just kept popping up that I never had before, and I just kept going to all different doctors.”
She went to Dr. Jaime Imitola, director of UConn Health’s Division of Multiple Sclerosis and Translational Neuroimmunology, for her neurological problems.
“She had Initial symptoms that are typical for neurological manifestation of long COVID like brain fog, cognitive decline, severe and persistent fatigue, headaches, all of which has improved significantly after our investigation and management,” Imitola says.
“I was very, very dizzy, and some of my walks were like crawls, to the point where sometimes I would just go around the block, and I didn’t know if I would make it home,” Beck says. “I had to go to physical therapy, cognitive therapy, and balancing therapy, as I had a few falls.”
She wrote notes to herself as reminders to complete routine tasks around the house, such as doing laundry, having breakfast, grocery shopping, and even taking a shower.
Davino recalls, “It got to points where we talked about, if things got worse, was she safe to live alone?”
“I felt like I had dementia,” Beck says. And there were more reminders for when she drove.
“I had Post-it notes that I would put in the car to tell me where I needed to go,” Beck says. “I’d put the directions for the post office, which literally is less than a half mile from my house. I would have to put the directions for all these places I went to daily.”
At another ED visit for of chest pain, she was sent to the Pat and Jim Calhoun Cardiology Center.

“She developed an abnormal heart rhythm called atrial fibrillation. This was causing her to have symptoms of tiredness and fatigue despite having an otherwise normal heart. She was treated with an ablation which has been highly effective in restoring and maintaining a normal rhythm, which has completely eliminated her symptoms,” says Dr. Christopher Pickett, interim director of the Calhoun Cardiology Center, who performed the ablation procedure.
“Everything I experienced at UConn was amazing,” Beck says. “I don’t normally go to the hospital. I’m a healthy person, so for me to go to doctor after doctor after doctor, that’s not normal. They were so kind.”
She would continue to experience that kindness when she returned as a patient for another matter.
“Every time I feel better, I start running,” Beck says. “In November of ’22, I felt better. I felt like my brain was coming back, so I started running again, instead of walking, just at a very slow pace. And then I had some stabbing pains in my stomach again.”
The abdominal pain was an example of a symptom that she would either ignore or forget about due to her memory difficulties. She would have to check her notes to realize it was a bigger problem than it seemed.
This time, the pain was followed by a fever the next morning, and it stayed with her long enough to compel her to seek care at a walk-in clinic near her home in Naugatuck. The staff there sent her to the hospital, and back to UConn Health she drove.
“I found out that I had diverticulitis, a small perforation [in the colon],” Beck says. “They hospitalized me for that, then I came home. And it happened again. I went, basically, back and forth in and out of the hospital.”

She became a patient of Dr. Eric Girard, who specializes in colorectal surgery.
“Dr. Girard, who’s another amazing person, who absolutely cares 100% about his patients, he took very good care of me,” Beck says. “He and his team were phenomenal. They answered my calls, they really worked with me to try to keep me out of the hospital and did everything they could.”
She would end up needing 18 inches of her large intestine removed.
“She had fevers, nausea, and severe abdominal pain, which are typical diverticulitis symptoms,” Girard says. “She was able to get better with antibiotics but then it came back again in April and we ended up doing surgery in mid-May [2023].”
Tears of Relief
By July, Beck had the green light to start running again.
“I never had tears from fear, and I think it’s because I had so much confidence in the staff, the team here at UConn, I just had so much confidence that they were just going to take care of me,” Beck says. “I had tears in my eyes two times during all of this. One was when I was told I didn’t have to come back [for a follow-up appointment] for another five years. I left and I thought, I’m going to be normal.”
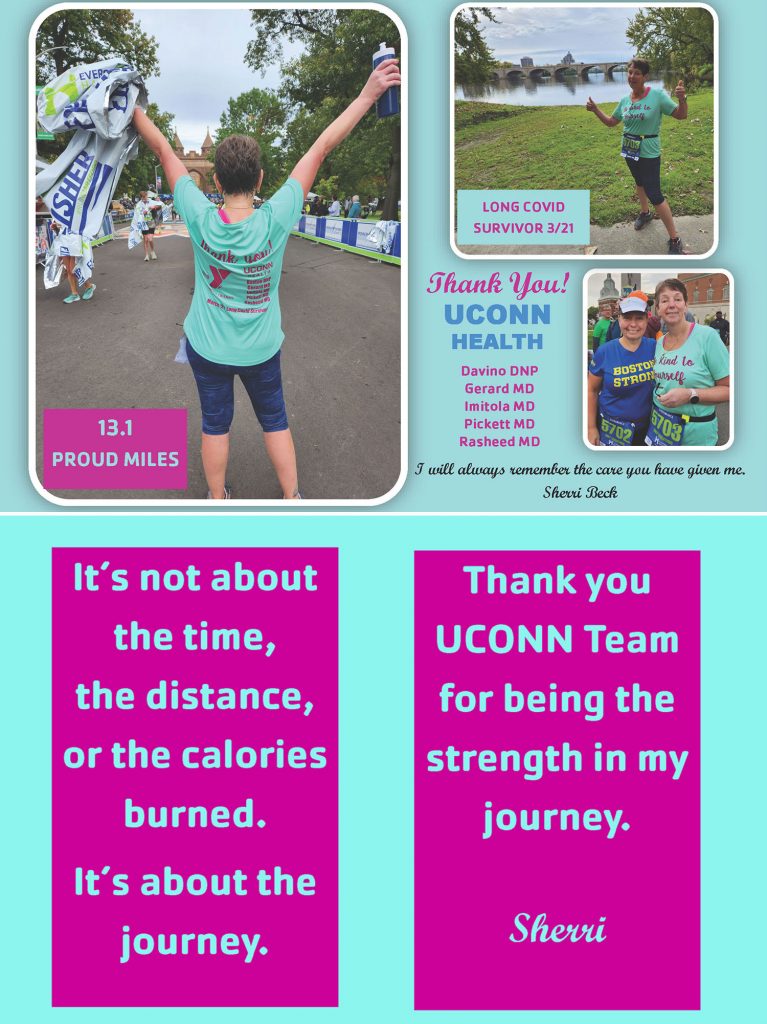
The other time was Oct. 1, at the 5-mile race at this year’s Southington Apple Harvest Festival, one of her favorites.
“Towards the end, I was talking with my sister, because she ran it with me, I was talking about how I went through a lot,” Beck says. “I just kept trying and trying and trying and trying, and now, I did it! I did the five-miler. I was a turtle. I don’t even care. I finished it.”
Beck says she still struggles with neurological symptoms and continues to see Imitola.
“She experienced these symptoms for almost two years but now she is back with improved cognition and ready to run marathons,” Imitola says. “Long COVID is still under investigation, and we know a lot about how the brain is targeted, however there are a variety of ways that COVID infection can attack the brain and a variety of disturbing symptoms that are coming to be recognized. Recently long COVID symptoms were added as a disability protected by the Americans with Disabilities Act. She is doing better, but we have many who are still suffering without significant improvements.”
Resilience and Gratitude
The story doesn’t end with the 5-mile race in Southington.
Two weeks later, something happened that would have been unthinkable in the previous two years: Beck laced up her running shoes for the Hartford Half Marathon.
“It was harder than the full marathon I had run,” she says. “I was even more of a turtle, but I finished it.”
Four days after she turned 54, and more than 2 ½ years since her last half-marathon, Beck went the full 13 miles.
“Sherri was determined to beat Long COVID from the beginning, and I am very pleased to see her back on running track,” Rasheed says.
Beck says now she’s working on strengthening.
“The care at UConn Health was phenomenal, and so I kept coming here with all the different scenarios that happened,” Beck says. “On my journey, when I was out there running, I just kept thinking, ‘You need to say thank you to this whole team you had.’”
She was insistent not only on saying thank you to her care team and all those whose work supported her care, but also on backing her words of appreciation with actions.
“I didn’t want my doctors, my nurses, the nurse’s aides, the housekeepers, anyone who was coming in to help me, thinking that I was just saying thank you. I made goodie bags,” Beck says. “It’s important to say thank you and show your sincere appreciation. I feel that it’s important for people to be aware of the quality care that the team is giving at UConn.”
Her gratitude may have been the one thing to outdo her resiliency. Or perhaps they worked together. Among Beck’s gestures of thankfulness were custom running shirts she had made. On the front was a reminder to “Be kind to yourself,” and on the back was a list of UConn Health providers whose care made her return to running possible.
“Tammy was my rock; she helped me out a lot and continues to help me, Dr. Imitola had a lot of patience with me, Dr. Rasheed was my knowledge, Dr Pickett educated me on my options and made my heart ready for my next race, and Dr. Girard was determined to get me to my surgery and guided me through it all,” Beck says. “I feel like I’m on my way to doing well, and you just have to thank those who were there for you. I am grateful for my team.”
Her focus now is to build her strength and speed, first with a 5K training plan, then 10K, and if her body continues to cooperate, a half marathon training plan, with an eye toward a faster time in the 2024 Hartford Half Marathon.
“She looks at herself every day, every half day, and it’s like, ‘How am I feeling right now? Can I keep going? Or do I need to stop?’ So I think that’s what she’ll do,” Davino says. “Start with a training plan, and if that goes well, build on it. And if it doesn’t go well, slow down, backtrack, maybe repeat that distance, that amount of mileage, and just go from there, and just wait until her body’s ready to move on.”