UConn Health is now a Huntington’s Disease Center of Excellence.
The Huntington’s Disease (HD) Program at UConn Health is honored with a new Center of Excellence designation by the Huntington’s Disease Society of America (HDSA) for its strong, longstanding multidisciplinary care team approach for Huntington’s Disease patients.
Sadly, HD is a genetic, rare, neurodegenerative disorder that runs in families with an incidence of nearly one case per 100,000 persons worldwide annually. If a parent is affected, there is a 50/50 chance of passing it on to each child. Unfortunately, many HD patients have already witnessed a parent, grandparent, or family member struggle severely or succumb to the inherited disease. There is no cure for HD, nor disease-modifying therapies, only various medications and psychotherapy counseling to treat the mild-to-severe HD symptoms as the disease progresses and is eventually fatal.
This new designation as a Center of Excellence is critical for Connecticut and its HD patients and their families. It will allow UConn Health to expand its patient care services and participate in more clinical trial research studies to find promising therapies such as new oral and injectable medications to slow the progression of the disease and eventually find a cure.
“When it comes to Huntington’s Disease, we are here to support the patient and the whole family,” says Dr. Shakaib Khan, medical director of the new HD Center of Excellence at UConn Health. “From initial education and counseling about the disease, to deciding whether or not to pursue anonymous genetic testing, to personalized treatments to manage individual symptoms, and planning for the future.”
During every clinic visit, UConn Health offers HD patients easy access to its full comprehensive services with expert care by psychiatry, neurology, social work, genetics, researchers, and other supportive professionals. Each patient and their family receive high quality care and individualized treatment plans throughout the course of their disease. In addition, UConn Health offers a Caregivers Support Group that meets virtually monthly.
The care team at UConn Health has extensive experience working with HD patients and their families. In fact, since 1998 UConn Health has been Connecticut’s first dedicated Huntington’s Disease Program. The HD program participates in the global Enroll-HD Study sharing its clinical research data with the world’s registry working toward finding new promising therapies and a future cure.
The Center of Excellence designation was made possible thanks to the team effort and leadership and dedication of Medical Director Khan, Robin Zingales-Browne, APRN, Andrea Gainey, MS, CGC, Genetic Counselor, Dr. Bernardo Rodrigues, Kristen Vavrek, MSW, and Sara Hatje, COA.
Medical Director Khan’s initial interest in specializing in Huntington’s Disease first occurred when he rotated through the clinic during his psychiatry residency training at UConn School of Medicine.
“As a young doctor in training, I was drawn to the intersection of both psychiatry and medicine at UConn as a psychiatry resident physician,” says Khan who was later fellowship trained in its integration. “I had a great experience as a UConn resident a decade ago to be a part of such an excellent HD program and patient lives. HD is a very complex disease and the most challenging of clinics I have been a part of.”
Khan returned to UConn Health as a faculty member in 2021 to serve as medical director for the HD program: “Our role at UConn Health is to hold the hands of our Huntington’s Disease patients as they go through their life’s journey. When it comes to the disease and its progression, we don’t have a magic wand or crystal ball to tell the future, but we help them maintain stability for as long as we can and offer the most supportive resources. Until there is a cure, we will help them lead the best lives possible.”
Thanks to the generosity of a philanthropic donor, anonymous genetic testing is offered to Connecticut residents who are at risk of inheriting the gene for Huntington’s Disease. All gene tests are done using strict confidentiality to ensure privacy for this vulnerable population.
UConn Health also has an established relationship with a long-term care facility experienced with the disease to assist its HD patients with an easier transition to this setting as their disease advances. The program’s APRN also visits the long-term care facility once a month to provide continuum of care.
“Our continued thanks for your support of the HDSA mission and all that you do to provide exemplary care to families impacted by Huntington’s disease,” said the award letter from the leadership of the Huntington’s Disease Society of America. HDSA has named UConn Health a HDSA Center of Excellence for three years and is awarding grant funding to expand its medical and support services for HD families.
“We have not lost hope for a cure,” says Khan. “Hope is still here. That’s why I am in academic medicine at UConn to pursue this interest. I love 100 percent of my job at UConn Health.”
Shining a Light on HD
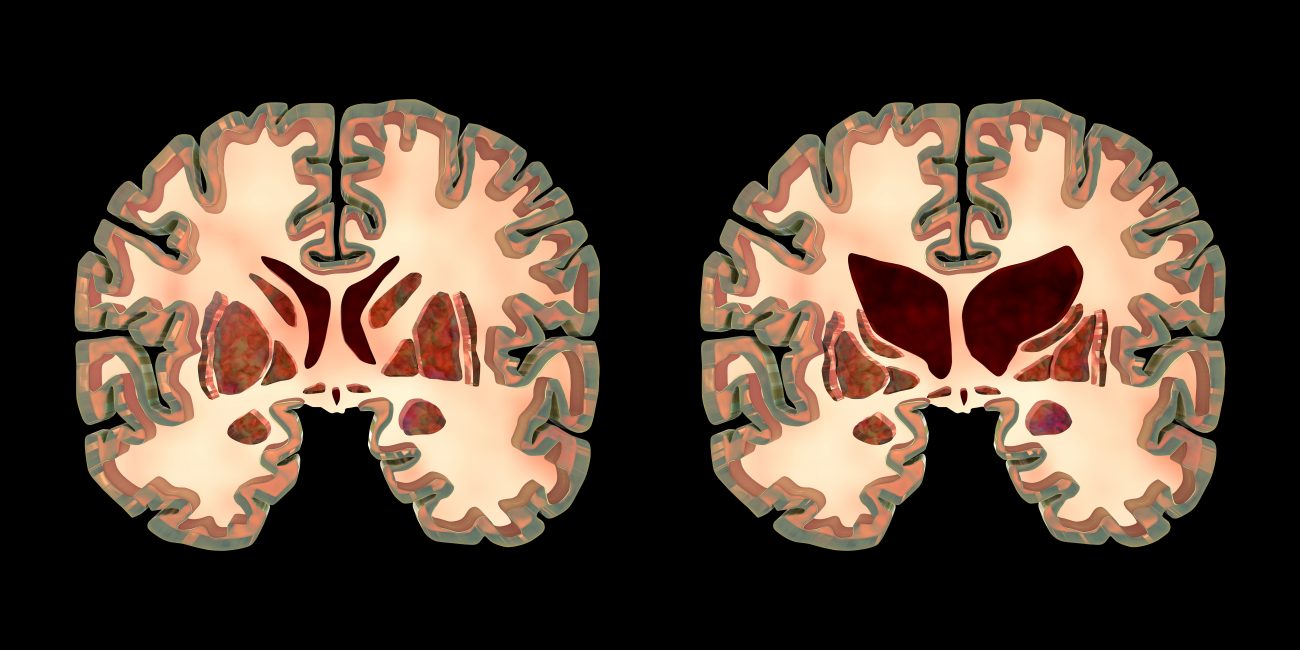
Huntington’s Disease is a neurogenetic condition. It is diagnosed through a simple, genetic blood test for assessing how many nucleotide (piece of DNA) repeats, referred to by the abbreviation CAG repeats a person has in DNA Chromosome 4. The higher the CAG repeats the worse the disease and faster the progression. We all have CAG repeats, but 26 CAGs or less is normal. There are two gray zones that do not result in HD, but only one gray that is important. The range of 36-39 is a gray zone where a patient may or may not develop HD. 40 CAG repeats or more causes patients to have symptoms of HD at some point in their lives. Unfortunately, the greater the genetic CAG repeats lead to over accumulation of mutant Huntington protein deposits in the brain causing neurons to die and wasting away of the brain’s cortex and striatum.
HD’s three, classic presenting symptoms can impact a patient’s motor, neuropsychiatric, and cognitive abilities. Secondary warning signs can present as weight loss, sleep disturbances, and autonomic dysregulation such as difficulty swallowing and unsteady gait.
HD-related motor function issues may appear as unpredictable involuntary muscle movements that are snake-like, or rigid muscles that affect walking and coordination.
Neuropsychiatric issues most commonly involve major depression (from 33% to 70% of patients), irritability (83%), apathy with lack of motivation (90%), suicidal thoughts (4 times higher rate than the general population) and suicide attempts (28%) just after diagnosis or as patients begin to lose independence.
Cognitive function impairments can slow a patient’s psychomotor skills like concentration and executive functions such as the ability to plan, stay organized, language skills, and memory.
While there is no typical HD case, onset of the slow-moving disease usually occurs between ages of 30 and 50 often lasting from 15-20 years with worsening, debilitating mental and physical symptoms. Rarely, 5% of HD cases occur in children and have more severe and rapid progression.
While there are currently two FDA approved medications for HD to help control involuntary movements, there are no approved treatments to stop the disease’s progression. In addition to medications used to treat HD patients’ varying symptoms, psychotherapy is a critical part of HD treatment to help patients manage their chronic, progressive, debilitating disease and elevated risk of suicide.
Patients or providers wanting to reach the HD Center of Excellence at UConn Health located at 5 Munson Road at the new Brain & Spine Institute can confidentially call: 860-679-6775.
The goal of the HDSA Center of Excellence (COE) program is to increase access to the best possible multi-disciplinary clinical care and services for individuals affected by Huntington’s disease (HD) and their families through a geographically diverse network of local and/or regional clinical centers.