Awareness about a disease in at risk-population improve outcomes.
That’s the simple idea behind a new, bilingual resource for both patients, medical students, and providers to help them overcome cultural barriers and recognize the early and critical symptoms of multiple sclerosis.
Social determinants of health, such as education, awareness, cultural, language, socio-economic or access obstacles, can cause unintended delays in diagnosing and treating MS, which result in patients missing out on timely interventions to avoid the onset of disability and progression.
Dr. Jaime Imitola, chief of UConn Health’s Division of Multiple Sclerosis and Translational Neuroimmunology, says the intention is to address a lack of education in medical students and general neurologists, and empower the community to remember the early signs of MS that require immediate attention.
“We have worked for the last five years to improve the care of the MS patients of the state of Connecticut, and we have created several strategies and research and build a national recognized MS center,” Imitola says. “In the last two years, with input of medical students, scientists and patients, we created a bilingual tool that collects, in a very clear, succinct manner, both compelling graphic and in words, the most relevant and alarming symptoms in early MS. We put it together in a framework that helps anyone to be educated about the initial red flags for multiple sclerosis.”
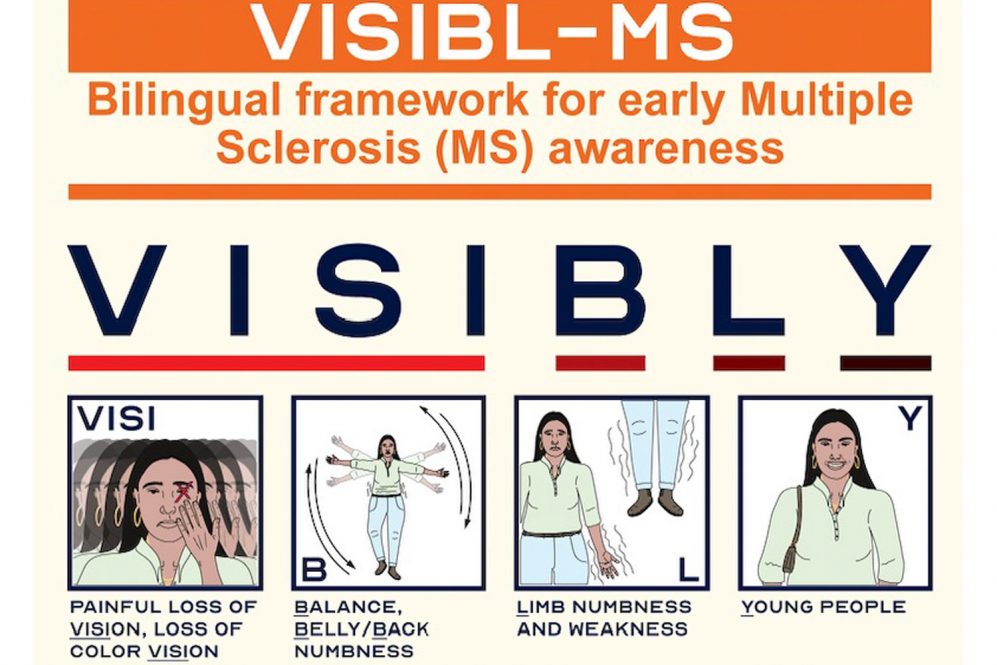
That led to the mnemonic “VISIBL-MS,” which is the basis for “VISIBLY” in English and “VISIBLE” in Spanish.
Spelling out the English example:
- VISI: Vision changes, including painful vision loss of color vision, or double vision
- B: Belly or back numbness or balance problems
- L: Limb weakness or numbness
- Y: Young people
Imitola reports on this novel framework in the Multiple Sclerosis Journal, a leading peer-reviewed publication in MS, with UConn medical student co-authors Shivam Patel and Seamus Rafferty and collaborators from Quinnipiac University in Hamden, Sacred Heart University in Fairfield, and the Lake Erie College of Osteopathic Medicine in Bradenton, Florida.
Noting how the acronym BEFAST has become synonymous with how to recognize signs of stroke, Imitola is hopeful VISIBL-MS will help the community identify people who may have early signs of multiple sclerosis.
As the authors explain, early MS symptoms are not often recognized by patients and general practitioners, and many patients are dismissed because of the transient nature of the initial symptoms or the belief that only Caucasian people get MS, only to come back with another attack contributing to delays in diagnosis and treatment.
“We hope to integrate our new tool into medical students’ education, but also that it can be helpful for patients and families, since the design is simple but very informative and the mnemonic can be used in English or Spanish,” Imitola says.
He notes that Connecticut has an increased prevalence of MS, around 370 per 100,000 people, “and there is enough evidence that diverse patients have worse MS due to intrinsic biological aggravated by social factors. UConn Health serves as the flagship safety net institution for the state and we need to make an effort to raise awareness in our populations that are minorities — African Americans, Hispanics, and others — because early awareness leads to early treatment and leads to prevention and changing the trajectory of the disease process.”
The VISIBL-MS tool is published as open access and free to all.
“These tools, developed by my team, encompass the strategic vision and identification of gaps in the real-world for our patients in Connecticut, harmonizing the mission of UConn Health, to bring solutions to the people of Connecticut through care, education and research,” Imitola says.