Dr. Justin D’Addario, vascular surgeon, and the vascular team at UConn John Dempsey Hospital are at the forefront of new innovative limb salvage techniques for severe and complex Peripheral Artery Disease (PAD).
On Jan. 25, D’Addario performed the first-ever alternative procedure in New England using DETOUR technology. Later, in May, D’Addario made history again by becoming the first in Connecticut to utilize the first and only FDA-approved drug-eluting resorbable scaffold, the Esprit Esprit™ BTK Everolimus Eluting Resorbable Scaffold System. Additionally, he was the first to use the Espirit BTK alongside DETOUR, combining both cutting-edge products for enhanced limb salvage outcomes.
The Esprit™ BTK Everolimus Eluting Resorbable Scaffold System (Esprit™ BTK System) offers a new option for people with the severe form of PAD for arteries below the knee.
D’Addario recently treated an 86-year-old patient with PAD who was in a critical situation: a non-healing wound on his foot, accompanied by significant leg and foot pain. With a 20-40% risk of losing the leg, the patient was already managing a prosthetic on the other leg due to a previous amputation. The innovative treatments employed by D’Addario and his team were crucial in addressing this severe condition and improving the patient’s quality of life.
Chronic limb-threatening ischemia below the knee is a severe form of PAD that occurs when arteries become clogged with plaque, preventing blood flow and oxygen from reaching the lower leg and foot. As a result, people living with this condition experience extreme pain, open wounds that don’t heal and, in some cases, amputation. Over a five-year period, this condition has a lower survival rate than breast, colorectal, and prostate cancer combined.
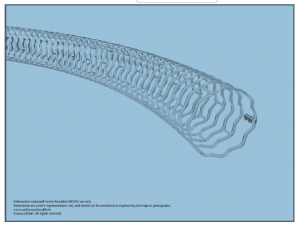
BTK Everolimus Eluting Resorbable
Scaffold System (Esprit™ BTK System)
offers a breakthrough option for people
living with chronic limb-threatening
ischemia below-the-knee.
Copyright: © 2024 Abbott. All rights
reserved. All trademarks referenced
are trademarks of either the Abbott
group of companies or their
respective owners.
The Esprit™ BKT System is a first-of-its-kind dissolvable stent for people with chronic, limb-threatening ischemia below the knee. Approved by the U.S. Food and Drug Administration (FDA) in April, the Esprit™ BTK System is designed to keep arteries open and deliver a drug called everolimus to support vessel healing prior to dissolving. The Esprit BTK System is comprised of materials similar to dissolving sutures. Once the blockage is open, the device is implanted through a catheter based minimally invasive procedure. The scaffold helps heal the vessel and provides support until it is strong enough to remain open on its own.
The new technologies represent a game-changer in the approach to treating patients with severe PAD. By combining this advanced technology with complementary systems, patients get a treatment option that has superior outcomes to standard care, while providing a less invasive alternative to surgery. This combined approach is particularly valuable for patients who are not suitable candidates for open surgery, ensuring they still have access to effective and innovative care.
“As an academic medical center, UConn Health is uniquely positioned to rapidly adopt and implement advanced treatment options. We are thrilled to offer minimally invasive solutions for patients with severe and complex Peripheral Artery Disease,” says D’Addario. “Our innovative approaches have already demonstrated successful, positive outcomes, and we look forward to continuing to make a significant impact on patient care by leveraging these cutting-edge techniques.”
While the Esprit™ BTK System is typically used as a standalone treatment, D’Addario’s goal for this high-risk patient was to exhaust all possible options to salvage the limb. This led him to combine Esprit™ BTK with the DETOUR technology. D’Addario envisions this integrated approach as setting a new standard of care in the coming years, offering enhanced outcomes for patients facing complex cases.
The DETOUR System, made by Endologix, won Breakthrough Device Designation from the FDA in 2020 and in June 2023 received FDA approval. Abbott’s Esprit™ BTK Everolimus Eluting Resorbable Scaffold System (Esprit™ BTK System) received Breakthrough Device Designation from the U.S. FDA in 2017 and was approved by the U.S. Food and Drug Administration (FDA) in April.
“The FDA’s approval of Esprit BTK System is a step forward in below-the-knee therapy. This new treatment option supports healing while reducing the risk of long-term complications,” says D’Addario. “We’re excited to be able to offer our patients the latest technological advancements to treat chronic limb-threatening ischemia below the knee.”
“The patient’s wounds healed within two weeks of the procedure, which is pretty remarkable,” says D’Addario.
UConn Health’s Division of Vascular and Endovascular Surgery specializes in the innovative treatment of aortic disease, peripheral arterial disease, carotid disease, mesenteric disease, and venous disease in patients of all ages. UConn Health surgeons are highly trained in the diagnosis, management, and surgical and endovascular techniques to treat these conditions, and they work closely with primary care providers as well as other specialists in vascular medicine, cardiovascular medicine, radiology, physical medicine, and rehabilitation to provide complete care.



