In the United States, breast cancer is the most common cancer in women, aside from skin cancer. The American Cancer Society estimates that in 2024, there will be about 310,720 new cases of invasive breast cancer in women.
But there is hope.
Advancements in early detection methods and support continue to increase the chances of survival. When caught in its earliest, localized stages, the 5-year relative survival rate of breast cancer is 99%.
Annual mammograms for those over the age of 40 and other imaging as determined by your provider is the key to early detection.
Terry Deely was diligent about her health and faithfully did all her preventative tests. So, in May of 2021 when she was diagnosed with breast cancer, she was shocked.
 “I was so surprised, my world crashed,” says Deely. “My sister and husband were with me, and I could see the doctor’s mouth moving but I could not hear what she was saying.”
“I was so surprised, my world crashed,” says Deely. “My sister and husband were with me, and I could see the doctor’s mouth moving but I could not hear what she was saying.”
All she could think was “how and why is this happening to me, I did all the right things.”
About half of breast cancers occur in women with no specific risk factors other than age and sex. However, a woman’s risk of breast cancer increases if she has a first-degree relative with breast cancer. About 5–10% of breast cancers are linked to gene mutations, such as BRCA1 and BRCA2.
Deely’s mother was diagnosed with breast cancer at 40 years old and had passed away from the disease at 47. Both of Deely’s sisters also had breast cancer.
She had a painful lump in her breast that led to an MRI that showed a fibroadenoma. A fibroadenoma is a non-cancerous, solid breast tumor that’s usually painless and feels like a marble under the skin. They are the most common type of benign breast tumor and are made up of glandular and connective tissue.
Advocating for herself, she told her doctor that she wanted it removed. Upon removal a 1.7 cm tumor was found hiding behind the fibroadenoma that had travelled to her lymph nodes. A biopsy concluded that two of the four nodes were cancerous.

Deely had a lumpectomy, and her breast surgeon referred her to oncologist, Dr. Yueming Chang to devise a treatment plan.
“The first time I met her, I left her office, and I said to my husband Pat, I know I am in good hands,” says Deely. “She is amazing and throughout the whole journey she was there.”
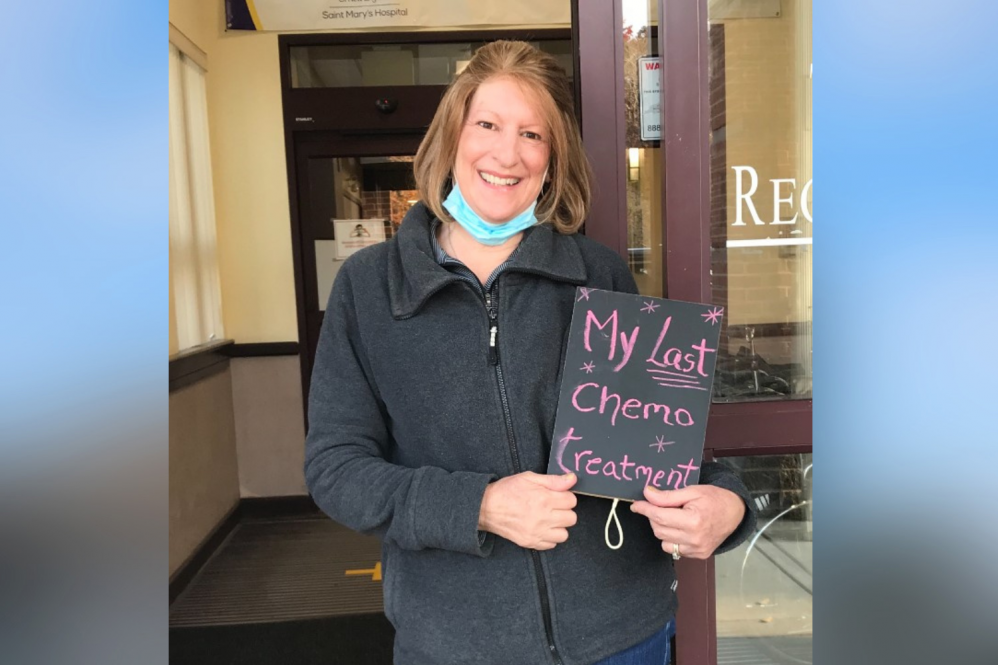
Deely had 16 rounds of chemotherapy and 21 rounds of radiation finishing chemotherapy in 2022. She had horrible side effects including mouth sores and brittle nails as well as the loss of her hair which was the hardest for her.
“If my hair doesn’t look good, I don’t feel good,” says Deely. “I hated wigs, but I lost all my hair, so I got a great wig and called it Amazing Grace.”
Each day as Deely went to work, which she did throughout her treatment, she would say “Grace lets go be amazing.” No one knew it was a wig until her hair started growing back.
When she heard Dr. Chang had left the practice she went to, she was disappointed and didn’t want to see anyone else. So, when she learned from a colleague that Chang was now practicing at UConn Health, she picked up the phone to see if she could see her and was thrilled when they booked an appointment for her.
“Honestly I love that woman, she is so good to me, so caring and concerned and always so positive,” says Deely.
Deely doesn’t mind the 45-minute drive from Watertown to Farmington to see Chang at UConn Health, “I’d follow her to the ends of the earth, I didn’t want to see anyone else.”
During her residency training, Chang’s mother who came to visit and help her taking care for her 2-month-old baby, started having some health issues and a colonoscopy detected colon cancer. For Chang, it was a harsh moment, she felt like she was in the medical field and didn’t know what to do. She leaned on her attending physicians and mentors for support, and her mother has since made it through and is now well.
Going through that experience made her want to help others knowing that patients and their family members need someone who understands when they get such a difficult diagnosis, and this led her to oncology as her subspecialty.
Chang joined the Carole and Ray Neag Comprehensive Cancer Center at UConn Health a year ago and has been helping patients with breast and lung cancer navigate their treatment.
“Early detection is very important, know your risk and going for screenings, you have a higher chance to cure the disease,” says Chang. “With advances in early detection and treatment options the survival rate is better compared to decades ago.”
In addition to a healthy diet, Chang encourages patients to exercise as physical activity helps reduce fatigue and exercise itself reduces the risk of recurring cancer.
“The prognosis and treatment are different for each patient, and here at UConn Health we individualize the patient’s treatment plan. Our multidisciplinary team considers genetics, tumor molecular changes, overall medical conditions, patient’s preference, psychosocial status to provide personalized care, ” says Chang.
Deely who is the clerical coordinator in the recovery room at a hospital sees this as her opportunity to be an inspiration to others and help them get through. She saw how hard her mother fought for her family, and she had to do it for hers. She is cancer free now and is regularly monitored.
“It’s a journey, everyone has the strength to overcome it. We are here to provide cancer patients the right support and care they need to navigate this challenging time, offering compassion and understanding every step of the way,” says Chang.
It takes a team to beat a breast cancer diagnosis and the team approach is the cornerstone of our breast cancer services at UConn Health. Every patient’s case and treatment program is designed specifically for the patient and is carefully assessed and frequently reviewed by a diverse team of specialists. In addition our breast cancer program offers support care services. To schedule your mammogram contact 860-679-2784.