At UConn Health’s Brain and Spine Institute, Orthopaedic Spine Surgeon Dr. Hardeep Singh specializes in some of the most complex spine surgeries performed today: from minimally invasive spine surgeries to complex reconstructive procedures for patients with spinal infections, tumor, deformities and failed prior surgeries.
These are not quick operations. They require hours of meticulous planning, advanced imaging, navigation, and often multiple surgical approaches. But for patients like Tina and Julie, the results are life changing.
Tina: A New Lease on Life
For Tina Krasniak, a nurse, spine problems had been a part of life for more than two decades. After multiple surgeries and bouts of sepsis at other hospitals, she was left with flat back syndrome, a severe spinal deformity that caused constant pain, loss of mobility, and the inability to stand upright.
“I couldn’t hold my upper body up anymore,” Krasniak says. “I was hunched forward all the time, looking up at people from their waist. Walking any distance meant leaning on a walker just to keep myself upright. Standing for more than a few minutes left me exhausted.”
Every aspect of her daily life was affected. “I couldn’t enjoy the active lifestyle I used to love such as raising and training Dobermans, golf and walking on the beach. Even simple tasks like cooking or shopping were too difficult,” she remembers.
Her turning point came when a nurse practitioner, Darcey Cusano at her community health center referred her to Singh. From the moment he reviewed her scans, Krasniak says she felt understood for the first time.
“From the moment he looked at my scans, he told me exactly what was wrong before I even said a word,” she recalls. “He was the first doctor who truly understood my problem.”
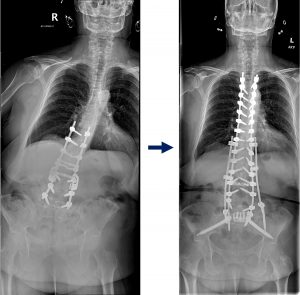
Singh diagnosed her with rigid spinal deformity and severe sagittal and coronal plane imbalance. The only way forward was a complex surgical reconstruction.
He explained every step of the operation: entering through her abdomen to remove old hardware, carefully breaking and realigning her spine, and reinstrumenting from her upper thoracic vertebrae (T4) to her pelvis (S2). The surgery would last more than 13 hours.
“He told me, ‘You’re not going to like me for a while, because this will be one of the hardest things you’ve ever been through,’” Krasniak says with a smile. “But he was right, and he was also right that it would be worth it.”
The recovery was grueling. Krasniak spent weeks in the hospital and rehabilitation facility before returning home. At first, she relied on a walker, then a cane. Her motivation came from a simple source her beloved Doberman, Sully.

“My goal was to walk him again,” Krasniak says. “He became my rehab partner, and he kept me going every day. Six months into my recovery he passed away and I adopted another Doberman from rescue, Phoenix, I’m not sure who saved who, but she kept me moving.”
Over the months that followed, Krasniak regained her independence. She began cooking, cleaning, and shopping on her own again.
Today, Krasniak can stand tall and walk without assistance. “I can look people in the eye again, without tilting my head up,” she says. “My lower back pain is gone. I feel like a completely different person.”
Krasniak adds, “He told me he could fix me, and he did. Dr. Singh and his team gave me my life back.”
Julie: Returning to the Life She Loves
Julie Diorio, 63, describes herself as a “busy body.” She loved hiking, gardening, and being on the move until her spinal deformity forced her into a painful, isolating reality.

Diorio first began experiencing unexplained neck problems two years ago. Despite worsening pain and visible changes her neck was even starting to bend forward toward her chest, her insurance denied multiple MRI requests. Eventually, after persisting with her neurologist, she received the scan that revealed a rare and serious infection in her bone. Doctors could not determine the exact cause or type of infection, even after extensive testing, but it required immediate treatment.
She underwent emergency surgery, followed by a long course of antibiotics that cleared the infection. Unfortunately, the damage it left behind in her cervical spine caused lasting complications. Julie went through multiple surgeries with different surgeons, but her condition didn’t improve — in fact, at one point it worsened. Finally, she sought out and was referred to Singh, a specialist who could address the complex damage to her neck and spine.
“I couldn’t do anything,” Diorio recalls. “I was embarrassed to go out. I couldn’t sleep in a bed, only on the couch, with three pillows stacked behind my neck just to keep my chin on my chest. I’ve always been active, but for months I was stuck inside. It was depressing.”
She had lived with these limitations for nearly a year before meeting Singh. She developed a chin-on-chest deformity and could no longer lift her head off her chest. She had to tilt her entire body backward just to look forward. He recommended reconstructive surgery to restore alignment and function. This would involve reconstructing her entire cervical spine to restore her ability to look directly ahead. The operation itself was just the beginning: the path to recovery would take months of healing and commitment.

“The road back would take time a year of follow-ups and patience,” Diorio explains. “I’ve seen him about five or six times since surgery. The follow-ups are so important. He checks that everything is healing correctly, that everything is in place. Each time I see him, I feel reassured.”
That reassurance gave her confidence to keep pushing forward in her recovery. She remembers the small but meaningful milestones standing taller, being able to walk outside again, and eventually returning to the trails she loves.
“Dr. Singh is thoughtful, compassionate, and he truly listens,” says Diorio.
Now, more than a year later, Julie is back to hiking and living the active life she feared she had lost forever. “I know I’m not going to be a perfect 10, but I’m not complaining,” she says with a smile. “Every day I’m a little stronger, and I’m grateful to have Dr. Singh guiding me through it.”
The Art and Science of Reconstruction
Cases like Diorio’s and Krasniak’s show the complexity of reconstructive spine surgery and why patients travel to UConn Health for Singh’s expertise.
These surgeries demand meticulous planning, advanced imaging and navigation technology, and often the removal or revision of prior surgical hardware. UConn Health is uniquely equipped to manage such challenges, with a multidisciplinary team that leverages cutting-edge preoperative imaging, surgical planning ehanced by artificial intelligence, state of the art intra-operative technologies, and surgeons specifically trained in complex adult spinal deformity.
Flat back syndrome, in particular, is a challenging condition that develops when the natural curve of the lower spine is lost, often after multiple prior surgeries. This creates a rigid deformity that forces patients into a stooped position, leading to severe imbalance, pain, and loss of quality of life.
“These conditions are not just about pain,” Singh explains. “They rob patients of independence, dignity, and the ability to live the lives they want. Reconstruction gives us the chance to restore not just their spine, but their hope.”
At UConn Health, advanced skill meets compassionate care. For patients like Tina and Julie, this means more than a straighter spine – it means the change to reclaim their independence, dignity, and lives. It is that blend of advanced surgical skill and compassionate, long-term follow-up that patients value most.



