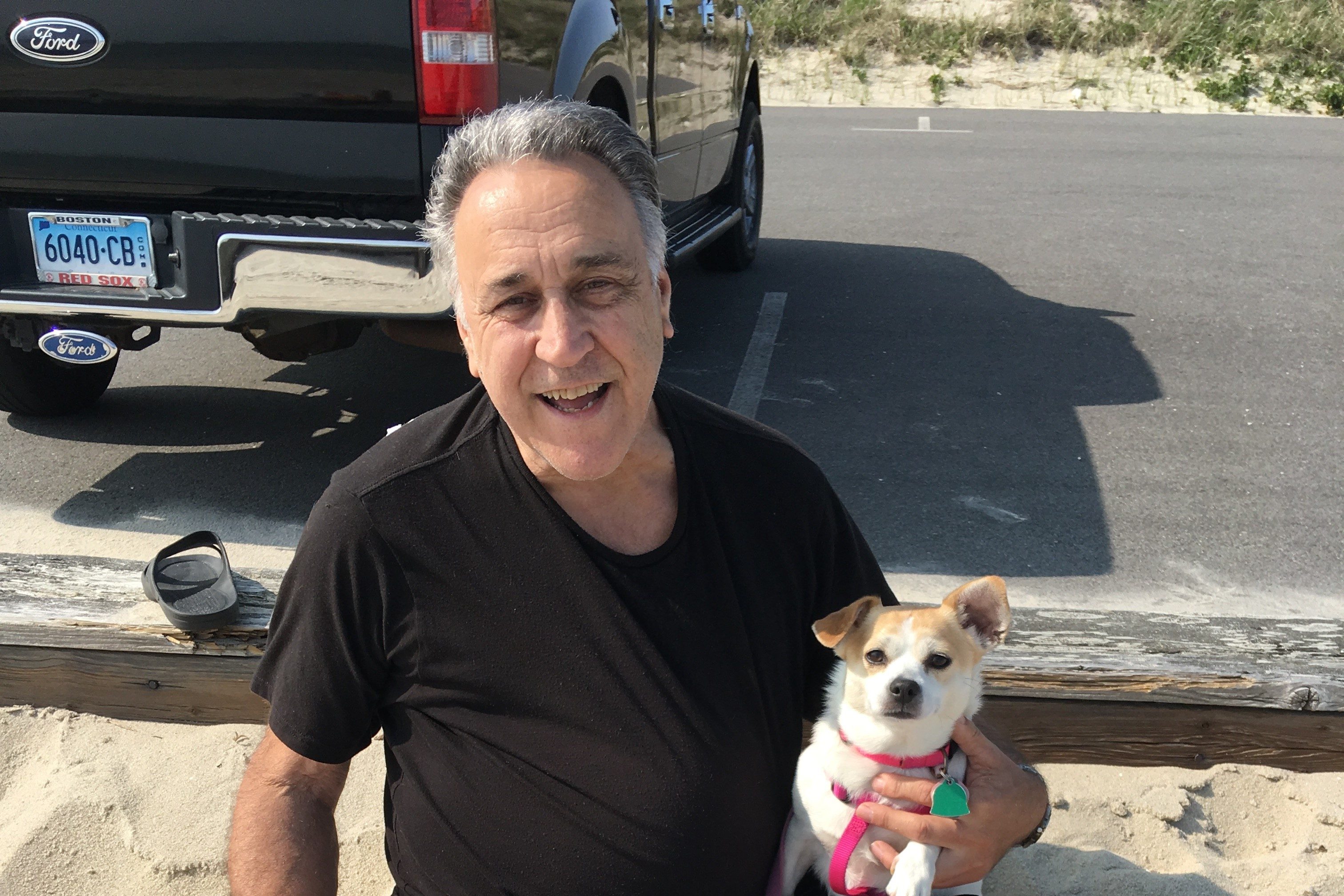
Michael Poulin, 70, of West Hartford woke up at 2 a.m. on July 1 with severe abdominal pain.
“I wondered if maybe I had something bad to eat?” he recalls.
Three hours later, unable to sleep and his abdominal pain worsening, he collapsed on to the floor from the pain. Thankfully, his wife heard him fall and called 9-1-1.
The ambulance brought Poulin to the Emergency Department at UConn John Dempsey Hospital, where a swift imaging exam confirmed that he had an abdominal aortic aneurysm (AAA), a ballooning of the aorta. It is the body’s largest blood vessel that carries blood from the heart to the chest and the lower abdomen.

The aorta is normally 3 cm or less in diameter. His aortic artery had enlarged to 14 cm and began to rupture.
Aneurysms are often referred to as ‘silent killers’ or ‘ticking time bombs.’ If identified early by doctors, they are monitored closely and surgically repaired before they get bigger than 5.5 cm, to avoid the danger of potential and often deadly rupture.
“Aortic ruptures have a more than 80 percent mortality rate,” says Dr. Jeffrey Indes, chief of the Division of Vascular Surgery at UConn Health.
Poulin says when the doctor showed him his medical scan, his ruptured artery looked like a “big round moon.”
Poulin had no symptoms or risk factors of an aneurysm prior to his sudden onset of abdominal pain – besides being a male over 60 years of age. However, in April 2015 he did experience some trauma to his chest during an automobile accident, from the severe jolt to his car and the force of a deployed airbag. He believes this chest trauma may have been the root cause of his weakened aorta.
Risk factors for aneurysm can include being a smoker, a family history of the disease, and high blood pressure. Often, the diagnosis of an enlarged or ballooning aorta can only be made via a vascular ultrasound screening by a primary care physician or vascular medicine expert.

Indes and his UConn Health vascular surgery team operated on Poulin right away, implanting the latest available endograft technology, made by Cook Medical. The flexible stent allowed surgeons to more quickly apply a seal to the aortic tear and stabilize the vessel to repair the rupturing aneurysm.
“This is one lucky patient,” Indes says, “and we are very happy to have been able to work together at UConn Health to repair his rupturing aorta quickly and have such a good patient outcome.”
Poulin is very grateful for the rapid, lifesaving emergency and vascular surgery care he received at UConn John Dempsey Hospital.
“You can’t do better than what they did for me,” he says. “I am very fortunate to have made it.
“From the paramedics at my home, to the ED, to Dr. Indes and all the nurses, there was a big team effort to get me to the OR,” he adds. “Through the whole process and recovery in the ICU and then the 5th floor of the hospital, they all are just the best. You couldn’t beat their care.”
After surgery, he recalls telling Dr. Dan Walker on Indes’s team, “I just couldn’t be happier!”
“I thank everyone, including the guy upstairs,” says Poulin.
Poulin was discharged home on July 4, just three days after the emergency aortic repair surgery, and now feels almost back to normal.

As a retiree, he is glad that he can simply follow his doctor’s orders to maintain his future vascular health.
“Dr. Indes told me I can go back to doing whatever I want to do! But of course nothing too strenuous and to walk as much as possible and often.”
There are three types of aortic aneurysms that can strike – including abdominal, thoracic, and thoracic/abdominal aneurysms – affecting the aorta and its supply of blood in both the chest and the abdomen.
“If you or a family member are over 60, have a family history, or have any of the aneurysm risk factors, talk to your primary care doctor about screening for aneurysm,” says Indes. “It could save your or the family member’s life.”