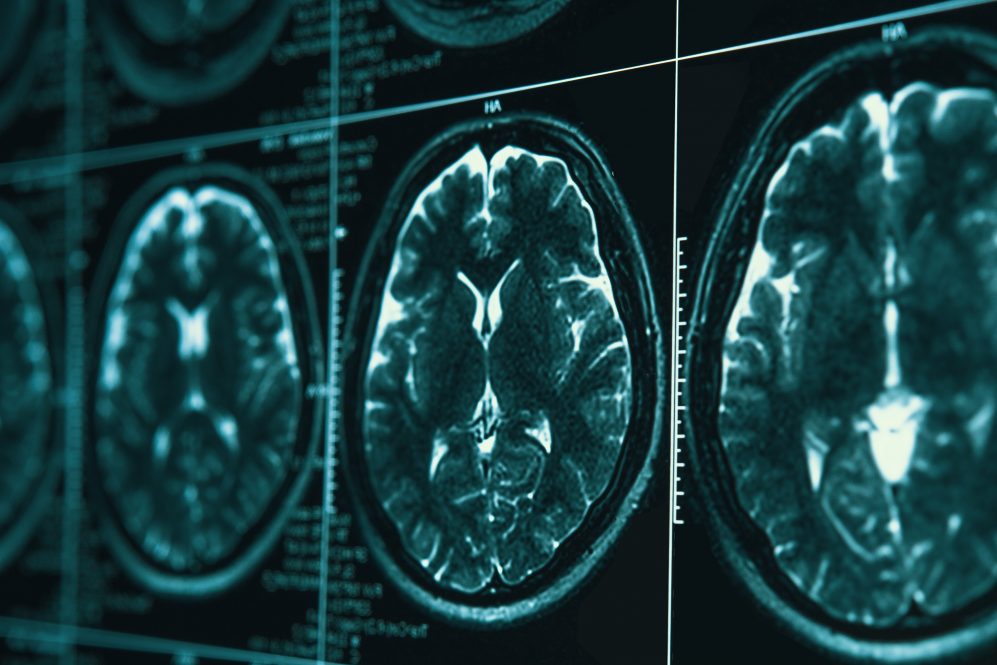
For decades, scientists have used brain imaging techniques – like PET scans or MRIs – to study psychoactive drugs. Antidepressant trials, for example, examine the brain of a depressed patient before and after taking the medication to help determine whether it is working as intended.
Sarah Feldstein Ewing, a clinical child/adolescent psychologist, had an idea to adapt this framework to study the effectiveness of another type of psychological intervention: therapy.
“What if we played snippets of therapy sessions back to people while they were in the scanner?” she wondered. “That could tell us a little bit more about how the brain changes in therapy.”
Feldstein Ewing, who joined the UConn Health faculty earlier this year as the Vice Chair for Research in the Department of Psychiatry in UConn School of Medicine, began testing this idea with adults and adolescents in therapy for addiction treatment.
Sure enough, she found that by measuring blood flow to different parts of the brain, she could determine which neural systems were being activated. Was it the reward system, associated with desire and habit-forming? Or the default mode network, associated with self-reflection and memory?
As these brain regions lit up, so did a new conclusion for Feldstein Ewing’s research.
She observed that the effects of therapeutic interventions on the brain were often reversed between young people and adults. In adults, the reward system was activated; in young people who received the same therapeutic intervention, the default mode network kicked into gear.
This makes sense, Feldstein Ewing explains, given the diverse motivations for substance use between teens and adults. Addicted adults are more likely to use drugs – even the caffeine in a daily cup of coffee – to stave off withdrawal effects, like the headaches and irritability that come from skipping a habitual morning joe.
“For adults, they are doing it because they know bad things will happen if they don’t,” Feldstein Ewing explains. “But kids don’t use in those kinds of ways. Kids use because they go to a party and there’s a ton of whatever – it could be vaping, cannabis, hard seltzers. They’re more exploratory.”
These findings suggest that different approaches are needed to help young people recover from substance use disorders and establish healthy coping mechanisms.
“I mean, these interventions were developed for adults, and we’re trying to shove them in, like ‘square peg, round hole’-ing them,” Feldstein Ewing says. “It doesn’t make sense.”
In the next phase of her research, Feldstein Ewing is looking to understand how clinicians can choose more effective techniques to support teen recovery. Using her novel MRI approach, she is exploring the efficacy of group therapy and new styles of motivational interviewing that have the potential to benefit countless young people.
“Historically, it’s been thought that teens are all doom and gloom, and that they’re never going to get better,” she says. “But I don’t think that’s the case.”
While there is a popular stereotype that teens are overly susceptible to peer pressure and desires to confirm, Feldstein Ewing spins this a different way, saying that teens are “very naturally socially gifted.” Because of this, peer-to-peer interventions and group therapy may be even more effective for this age group than for adults.
“Teens can very quickly evaluate what’s happening socially and can modify their behavior accordingly,” Feldstein Ewing says. “They are flexible, in these very savvy ways that you lose as you get into adulthood. So, we’re trying to figure out how to harness and enhance some of these natural gifts.”
A Career of Care
Feldstein Ewing has long been interested in adolescent development and addiction recovery. Growing up, she says, “I had a lot of friends who happened to really get waylaid by different kinds of drugs. It was just so confusing to me, how these amazing, vibrant kids could just get derailed.”
She studied neuroscience at Macalaster College in Saint Paul, Minnesota, received her Ph.D. at the University of New Mexico, and embarked on postdoctoral work at Brown University, all the while pursuing answers to the questions of “what can the brain tell us about why people sometimes make terrible decisions, and how can we get people back to their best selves?”
Prior to joining the UConn Health faculty, Feldstein-Ewing was a clinical psychology professor at the University of Rhode Island (the College of Health’s endowed Prochaska Professor of Population Health). Before that, she taught as a professor of psychiatry at the Oregon Health and Science University (OHSU) and directed the Adolescent Behavioral Health Clinic at OHSU Doernbecher Children’s Hospital.
While in Oregon, she helped launch the groundbreaking ABCD (Adolescent Brain and Cognitive Development) study, the largest-ever cohort study of teen brain development. It follows over 10,000 healthy children from ages 9-10 through adulthood, tracking how their brains develop, and how this process is influenced by personal and global factors – such as drug use or a pandemic. Now in its ninth year, the ABCD study is providing vital new data for researchers across various fields.
In her new role as the Vice Chair for Research in UConn Health’s psychiatry department, Feldstein Ewing is eager to use her impressive background to help support research development efforts across the school.
“I have a special eye toward helping women and underrepresented scientists,” she notes.
And as her personal scholarship progresses, she hopes to continue making a difference in the world of addiction treatment and recovery. If there’s one thing she’s learned from years spent studying the brain, she says, it’s that there is always hope for flexibility and change.
“The brain has a lot more capacity for recovery – even moment to moment – than we may have thought,” she says. “People don’t necessarily have to stay stuck in these entrenched systems forever. They can get better. They can be resilient.”