UConn Health is offering a new standard of care for patients who’ve suffered the most common type of stroke. UConn John Dempsey Hospital is among only a few hospitals in the state to offer a specific cutting-edge neuroimaging technique that involves new software called “RAPID.” It facilitates computed tomography (CT) perfusion imaging in emergency settings by making radiologic interpretation of perfusion data simpler, a particularly crucial feature when treating emergency stroke patients.
This helps physicians determine which patients are good candidates for a highly specialized neurosurgical and interventional radiological procedure called mechanical thrombectomy.

For stroke patients it means the narrow window for intervention potentially quadruples, to 24 hours from the onset of symptoms.
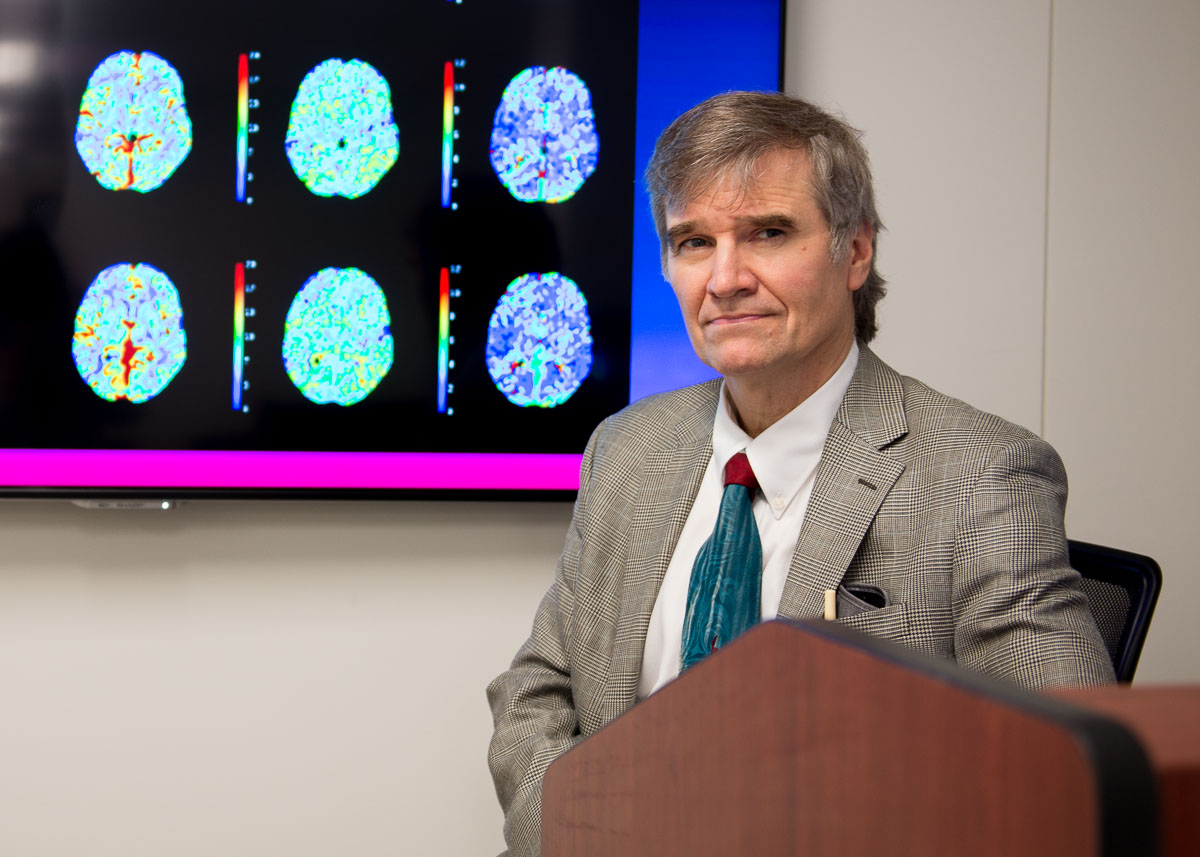
“It enables us to easily check how large an area of the brain is deprived of blood flow,” says Dr. Leo Wolansky, who arrived as chair of the UConn Health Department of Radiology in March. “We can distinguish between the part of the brain that’s already dead (cerebral infarction) and the part of the brain that is in danger of dying (ischemic) but can be saved.”
UConn Health rolled out its perfusion imaging program just this month after the arrival of the RAPID software. A week earlier, UConn Health processed its first functional MRI case for surgical guidance. The innovations are part of a system-wide initiative by UConn Health leadership to provide cutting-edge technology and recruit top physicians familiar with its use, such as Wolansky, in order to provide the finest care for neurological conditions, such as stroke.
Dr. Sanjay Mittal, medical director of the UConn Health Stroke Center, credits two other key additions to the faculty, co-director, Dr. Gracia Mui, and Dr. Ketan Bulsara, chief of the Division of Neurosurgery, with helping the stroke program make great strides this past year.

“The arrival of Dr. Bulsara and Dr. Mui, along with the implementation of RAPID, enables us to provide the best care for complex stroke patients,” Mittal says. “UConn Health prides itself in shared decision making between patients, their families, and clinicians.”
When Bulsara arrived in May, he brought an elite capability to offer several highly specialized cranial procedures, including mechanical thrombectomy.
“The stroke program in many ways is the epitome of personalized collaborative care that UConn Health offers,” Bulsara says. “It is a multidisciplinary team with one goal, to optimize patient outcome. Dr. Mittal started to lay the foundation for this and we are all fortunate that we get to continue building on it. Dr. Wolansky’s commitment to provide state-of-the-art neuroimaging makes us one of the few centers that are in an amazing position to appropriately select patients who would benefit from mechanical thrombectomy.”
Historically when a cerebral infarction, the most common type of stroke, happens, the race is on to administer a clot-dissolving medication known as a tissue plasminogen activator (TPA). Mechanical thrombectomy traditionally has also been an option with a very limited timespan. With the introduction of advanced imaging such as RAPID, patients now can be treated safely for up to 24 hours of their stroke if the CT perfusion scan is favorable.

“We can tell if there is brain that can be saved, even beyond the previously accepted window of time for thrombectomy,” Wolansky says. “This creates the possibility of treating many ‘wake-up’ strokes, people who went to sleep well, but woke up eight hours later with a stroke.”
The value of perfusion imaging with RAPID to guide thrombectomy selection has grown significantly since May. That’s when the results of a major study known as the DAWN trial showed good outcomes for stroke patients who were treated with thrombectomy – in the window up to 24 hours after the event. It followed patients for three months after suffering a stroke, and found the thrombectomy group to be four times more likely to be functionally independent than the group that was not treated with thrombectomy.
“To manage your own activities of daily living, that’s a goal everyone wants,” Wolansky says.
More information about the UConn Health Stroke Center is available at health.uconn.edu/stroke-center.