Researchers at the University of Connecticut Health Center presented a videoconference workshop Thursday to explain and promote genome editing, a pioneering technology that may lead to new treatments and cures for devastating conditions such as cancer and autism.
“This recent advance is the first generation of new technologies for personalizing stem cells,” says Marc Lalande, professor and chairman of the Department of Genetics and Developmental Biology. “Gene editing will allow us to create cell models for large numbers of diseases. The applications are limitless.”
In the past, researchers have studied disease on a cellular level by comparing cells from a person with a certain condition to cells from a healthy individual. But this approach “was like comparing apples to oranges” because of the inherent genetic differences between two people, Lalande explains. “There are millions of small differences, which makes it difficult to really study disease.”
Genome editing involves a cut-and-paste approach in which an individual stem cell line is modified to create a cell line that contains a new disease-causing mutation. Alternatively, one can start with a cell line that has a genetic defect, cut out the abnormal DNA, and then paste in a correct copy to repair the defect. In either case, the new cell line is genetically identical to the starting cell line, except for the change that has been engineered. “So now we can compare apples to apples,” Lalande explains.

By efficiently making changes to the DNA of human cells, researchers are creating models that can be used to study a wide array of diseases. One example, Lalande says, involves the study of post-traumatic stress disorder (PTSD). The predisposition or risk for PTSD is associated with two factors – childhood trauma such as abuse, and genetic variation in the FKBP5 gene.
Health Center researchers have created a human embryonic stem cell line that carries the risk variant for the FKBP5 gene as well as one with a protective variant. They then use drugs to stress the cells in culture and analyze the results. That one change to a single nucleotide could hold the key to understanding why some people are more susceptible to PTSD than others, and this could lead to better treatment options.
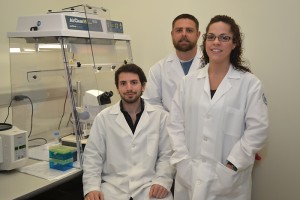
In a presentation at the workshop that focused on modeling cancer, Christopher Heinen, associate professor of medicine at the Neag Comprehensive Cancer Center and Center for Molecular Medicine, and director of UConn’s Molecular Biology and Biochemistry Graduate Program, discussed the role of genome editing in the study of hereditary cancer.
“Cancer is a disease of genetic mutations,” he points out. “Any particular cancer can have a number of different mutations. Our goal is to isolate one specific mutation at a time, to determine what it does in the cell.”
This information can reveal whether a person who has such a mutation is at a higher risk for cancer, which in turn could lead to earlier screening or preventive therapies. The focus of his studies is colon cancer, but the genome editing technique can be applied to studies of other types of hereditary cancer, such as breast and endometrial.
“I certainly think we’re at the cusp of understanding the genetic complexity of cancer,” Heinen says. “Now as cancer genomes are sequenced, we are seeing the larger picture and learning that there are a lot of genetic differences. But we are searching for similarities too.”
Identifying pathways that are similar can lead to combination therapies to attack cancer in two ways – a general treatment and a personalized one designed for each particular case. “The idea of personalized medicine really applies to cancer because it requires an individualized approach, but there also may be overlaps in treatment that we can identify.”
Also discussed at the workshop were genetic models of autism as well as Marfan syndrome, a connective tissue disorder that can cause serious eye, joint, and heart problems. The overall goal was to share knowledge with other investigators on how these cutting-edge technologies can benefit their research program and how to access them.
Genome editing “is a marriage of genomics and stem cell technology,” Lalande says. “It’s in keeping with the Bioscience Connecticut initiative and the genomics partnership with Jackson Labs.” These ventures are part of the state’s effort to bolster its economy by supporting biomedical research to create jobs and secure the Health Center’s future as a top academic medical center.
“We have developed some new ways of making stem cell models, and the purpose of the workshop was to let the research community know that we have this technology in place and what they could do with it,” says Lalande. “Genome editing is very cool – there’s no other way to say it. It’s remarkable.”
Follow the UConn Health Center on Facebook, Twitter and YouTube.