Prostate cancer is the second deadliest cancer in men in the U.S. It kills more than 26,000 men in the country every year. But, as in the case of breast cancer, one prostate cancer will progress rapidly while another tumor will sit for decades and never spread. In the March 14 issue of Science Signaling, UConn Health researchers describe how a well-known protein might reveal whether a tumor is mild-mannered or out to kill.
Researchers have known about prostate-specific membrane antigen (PSMA) for more than 30 years. Yet they weren’t sure what it did. They knew there’s not a lot of PSMA on normal prostate cells, but as the cells become cancerous, growing faster and starting to invade surrounding tissues, more and more PSMA appears on the tumor cells. Recently, two UConn cell biologists, Leslie Caromile and Linda Shapiro, wondered what the PSMA was actually doing. Did it help the cancer cells get worse in some way?

To find out, the two researchers at UConn Health bred mice that tend to develop prostate tumors to other mice, that were identical save that some could and some could not make the PSMA protein. The offspring developed prostate tumors either with or without PSMA. The tumors in mice that lacked PSMA were much less aggressive, with a more limited blood supply, than the tumors grown by their PSMA-making siblings. In other words, the PSMA-free tumors were much less cancerous.
The researchers then looked at cell lines developed from human prostate tumors to see if the observation held true for humans as well as mice. They removed the ability to make PSMA from some cells and compared them to their parent cells that still had PSMA. Importantly, the human cells without PSMA acted just the same as the mouse tumor cells lacking PSMA, confirming that PSMA worked the same in lab mice tumors as it did in human prostate tumors.
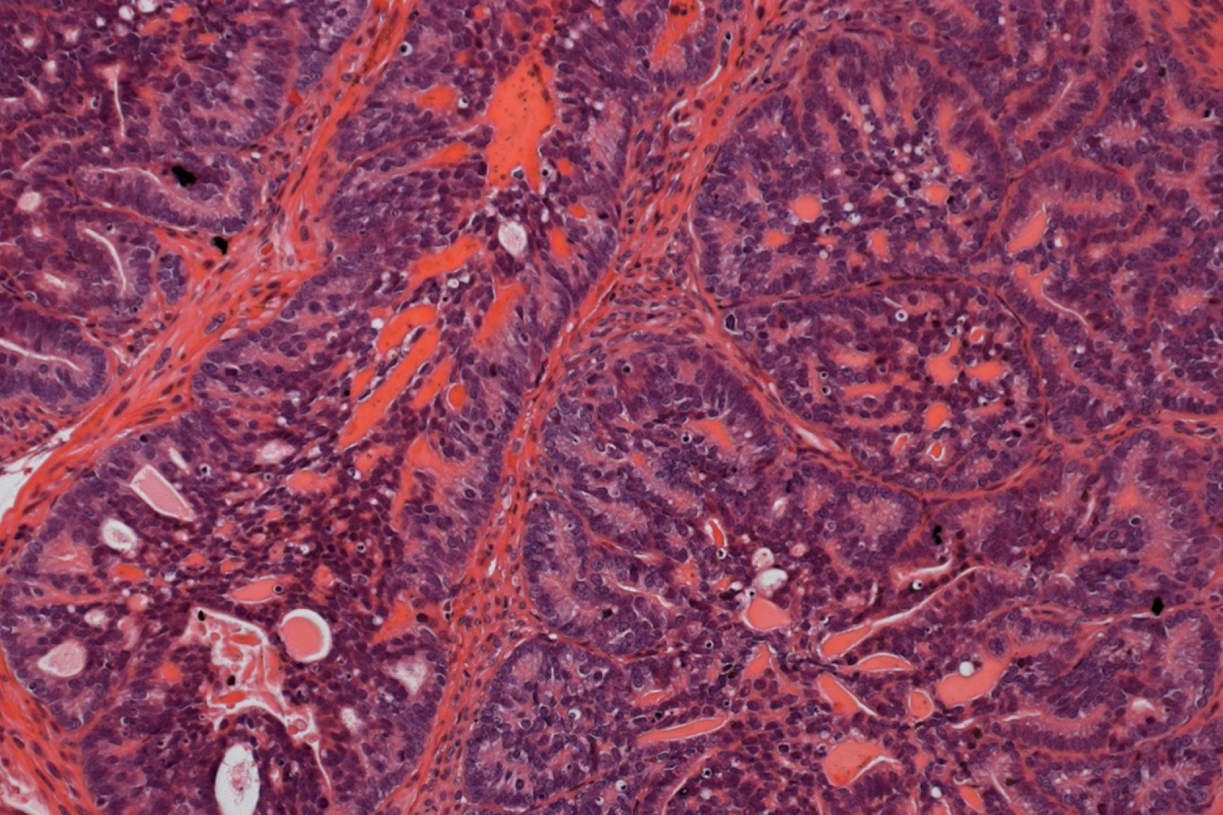
Caromile and Shapiro then examined databases characterizing over 50 human prostate tumor biopsies. Each biopsy was rated for tumor aggressiveness and how far the cancer had progressed. The researchers found that all of the biopsies rated as more aggressive had more PSMA than the biopsies rated as less aggressive. Some of those were also matched with benign, non-cancerous tissue donated by the same person – and in every case, the benign tissue had little or no PSMA compared with the cancer. It was clear that PSMA is tightly linked to prostate cancer. But why?
“We found that PSMA changes signals inside the cell to make cells grow faster, resist stress better, and survive longer, as well as be less sticky and probably metastasize faster,” says Shapiro. The less that cells stick to one another, the more likely they are to detach from the main tumor and travel around the body to form other tumors. PSMA also appears in other cancers driven by hormones, such as endometrial and breast cancer, as well as in bladder cancer. Caromile and Shapiro’s next set of experiments will explore how PSMA is related to metastasis, the process of cancer spreading throughout the body. It is actually the metastases that are the big killer in prostate cancer, and so finding more about how PSMA regulates their signals would also benefit patients.
Proving that abundant PSMA on a cell’s surface goes hand-in-hand with cancer opens up many new opportunities, Caromile says. PSMA is already used as a target for delivering chemotherapy, but could be a good drug target itself. Because it seems to be activating pathways that make cells cancerous, shutting down PSMA might shut down a cancer. Although using it as a drug target is still far off, it’s a promising lead that could help doctors and patients narrow the uncertainty when deciding how aggressively to treat a tumor. And eventually, drugs that disarm PSMA could change the very nature of a tumor from a killer to a mere annoyance.