[yframe url=’http://www.youtube.com/watch?v=mtnliHX4M2Q’]
Scarred by years of torture and abuse under the brutal Khmer Rouge regime, Cambodian refugees in the United States have been found to have significantly higher physical and mental health problems compared to the general population.
Helping them address their health issues and receive sustained, adequate health care hasn’t been easy. Many of the refugees view Western medicine as complementary to traditional Cambodian healing practices – which may include Buddhist healers, herbalists, and acupuncture – and only visit a primary care physician infrequently. Language barriers, social isolation, lack of access to transportation, and limited financial resources create further impediments to receiving quality care.
In response to the problem, two UConn professors are working to improve the health outcomes of Cambodian refugees through community outreach, medication therapy management, innovative telemedicine and technology services, research, and policy changes.

Thomas Buckley, an assistant clinical professor in the School of Pharmacy and an expert on health disparities and access to care, has been working with a Connecticut nonprofit advocacy group for the past seven years to make sure older Cambodian-Americans in Connecticut, Massachusetts, and California are taking the medications they need. In addition to serving as a clinical consultant for Khmer Health Advocates (KHA) of West Hartford – the only Cambodian-American health care organization in the U.S. – he is preceptor of a clinical rotation for UConn pharmacy students involving Cambodian refugees.

On another front, S. Megan Berthold, assistant professor of social work and an expert on the physical and mental health consequences of trauma in refugee groups, has spent the past 12 years working with a team of researchers to identify Cambodian refugee physical and mental health problems through an NIMH-funded initiative undertaken in collaboration with the RAND Corp. The project is led by Grant Marshall of RAND Corp.
Berthold also recently started working with the KHA, where she oversees a UConn-funded community-based participatory research study for Cambodian-Americans that uses computer tablet technology and native language software to assess the health needs of Cambodian-American communities in six cities around the U.S.
Bridging the cultural gap
As part of the clinical rotation program Buckley manages at the KHA, UConn pharmacy doctoral students work side-by-side with Cambodian community outreach workers to assess the health needs of Cambodian refugees and help them manage their medications. The students participate in face-to-face visits with Cambodian-Americans in Connecticut and Massachusetts, and help counsel individuals in California through advanced video teleconferencing. Long Beach, Calif. has the nation’s highest population of Cambodian-Americans, with more than 70,000 residents.
“Cambodian-American health outcomes are especially bad because of the treatment they received under the Khmer Rouge,” says Buckley. “Their rates for diabetes, hypertension, depression, and other symptoms associated with post-traumatic stress disorder are much higher than other groups. Although the genocide of the Khmer Rouge happened 30 years ago, the after-effect is still manifesting itself now.”
The UConn pharmacy students use a specially-developed questionnaire to assess a person’s medication and health problems. The information is then shared with a licensed pharmacist, who may recommend dosage changes, alternate treatments, or other action. The students in the program get first-hand experience with medication therapy management, cultural competency training, and community pharmacy practices.
“We are exploring innovative ways pharmacists can work with a community health worker and bridge the cultural gap in order to provide better health services,” says Buckley.
“The biggest problem we see is the complexity of the therapies,” he says. “A lot of people are getting their drugs from many different sources. They don’t have one primary care physician controlling everything. Because they have poor access to healthcare, they are getting their drugs from a spouse, a sister, an uncle, a close friend … we found people were taking multiple drugs that were doing the same thing.”
Some of the nearly 100 Cambodian-Americans surveyed through the program had stopped taking certain medications after experiencing adverse side effects. Others took too much medicine, resulting in additional health concerns.
As a result of the pharmacist-community worker intervention, successful therapy outcome goals increased from 69 percent to 93 percent among program participants over a 12-month period, inappropriate medication use declined by 35 percent, and medication adherence improved 23 percent. A review of the program’s return on investment projected that for every $1 associated with the cost of the program, $6 in health care savings was returned.
Buckley’s work led to his receiving the Connecticut Pharmacists Association’s 2012 Excellence in Innovation award for outstanding advancement of pharmacy practice. He received the UConn Provost’s Award for Excellence in Public Engagement in 2011.
Documenting physical and mental health problems
Berthold, meanwhile, recently entered the second phase of a major research initiative involving the health and well-being of Cambodian-Americans. She is part of a team of researchers at the RAND Corp. that is documenting the prevalence of physical and mental health problems among older Cambodian-Americans and examining whether there are any links between trauma, post-traumatic stress reactions, and chronic health problems.
Berthold says the longitudinal study with RAND has amassed a large amount of data. “The U.S. Veterans’ Administration is very interested in chronic health issues and the possible link between PTSD and depression and chronic physical health problems such as cardiovascular problems, high blood pressure, and diabetes. We are examining those issues in Cambodian-American survivors of the Khmer Rouge Killing Fields.”
The RAND study was the first prevalence study of mental health problems in a random sample of Cambodian-American survivors of the Khmer Rouge genocide. Initial findings were published in the Journal of the American Medical Association in 2005. As part of the second wave of research, Berthold is looking at long-term mental and physical health issues in the sample population, and, in a separate study, the mental and physical health of Cambodian-American youth born in the U.S.
Building capacity
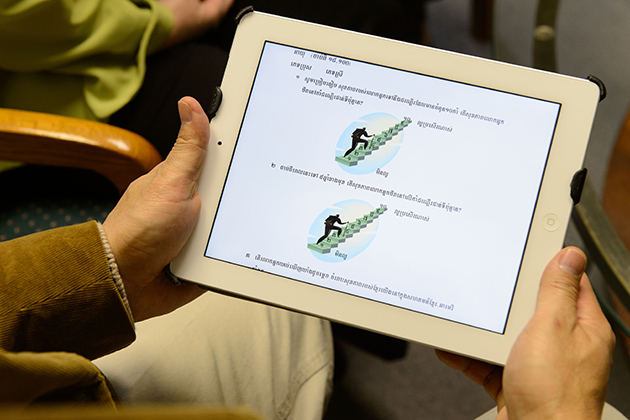
Berthold is also the principal investigator on a community-based participatory research project in partnership with KHA and Cambodian NGOs around the country. KHA project director SengLy Kong is co-investigator. The study, funded by a UConn Faculty Large Grant, involves testing the feasibility and effectiveness of training Cambodian community health workers to collect data using iPad tablet computers.
The project aims to gauge Cambodian-Americans’ concerns about the health of their communities, as well as their perceptions about barriers to effective healthcare. Community members are able to interact with the devices in their native Cambodian language Khmer. The results will be interpreted by Cambodian-American community leaders around the country who are partners on the project, and used by the community to develop a comprehensive plan to reduce health disparities and improve health outcomes in this population.
Cambodian-American health outcomes are especially bad because of the treatment they received under the Khmer Rouge. … Although the genocide of the Khmer Rouge happened 30 years ago, the after-effect is still manifesting itself now.
“We are trying to build capacity in the Cambodian-American community across the country to conduct research and address the significant health disparities they face,” says Berthold, who was named the National Association of Social Workers 2009 Social Worker of the Year. “Cambodian-American leaders from six states who run Cambodian-American NGOs have collaborated as partners in the development and implementation of every stage of this project. We plan to share the data through telephone conference meetings, and ask for stakeholders’ help in interpreting the data and identifying a focus for further research that is meaningful and important to the Cambodian-American community.”
UConn experiential education field coordinator Lisa Bragaw and associate clinical professor of pharmacy Devra Dang are assisting with the research, as are UConn Health Center licensed clinical psychologists Julie Wagner and Elizabeth Schilling, and Thiruchandurai Rajan, professor of pathology and laboratory medicine.
Mary Scully, programs director for KHA and an advanced practice registered nurse, says the work is greatly appreciated. “I think having pharmacists more involved in health care is a very practical solution to helping people with their medical problems,” she says. “The pharmacists in our program have done a great job talking with the community. They are very knowledgeable, and the community really picked up on that. They loved the service and when they saw the drop in the depression rate, it seemed to really empower them.”