The first Ebola case in West Africa may have appeared in a 2-year-old boy in Guinea in December 2013. It then spread to neighboring Liberia and Sierra Leone. By March this year, health care workers were aware that a regional outbreak was underway. But it was an American’s death in July that woke the world to the epidemic.
Patrick Sawyer was a U.S. citizen working for the Liberian government who traveled by air to Nigeria while experiencing symptoms of Ebola. He collapsed in the Lagos airport and died in hospital five days later. The fact that he arrived in the capital city by air alarmed many about the possibility of global consequences.
This outbreak is larger than any previous and, as of this moment, it is still expanding. This disease is surrounded by mystery and frightening images, both real and fictional. Professor Kenneth Noll in the Department of Molecular and Cell Biology offers a true picture of Ebola and the potential consequences of the West African outbreak.
The West African outbreak is the worst recorded incidence of Ebola. Ebola first came to the attention of Western medicine in 1976, when an outbreak of a hemorrhagic fever took place in the Democratic Republic of the Congo (then called Zaire). Until the current outbreak, it had only occurred naturally in Central and East Africa. Cases appeared elsewhere as the result of laboratory contamination or export of infected monkeys used for research. Prior to the current outbreak, the most deadly episode was the one in 1976 in Zaire, when 280 people died, representing 88 percent of those known to have been infected.
Those outbreaks were smaller because the disease is typically found in rural areas that have low population density. By contrast, the West African outbreak occurred in rural communities that are much closer together, where people frequently travel among neighboring communities.
Medical professionals in East and Central Africa have become familiar with Ebola since it has been known in those areas for almost 40 years. Medical providers in West Africa were less able to identify the disease when it appeared, and so precautions to prevent its spread were not immediately implemented. Medical facilities there also typically lacked the simple protective materials–gloves, face masks, and gowns–necessary to protect doctors and nurses, so medical providers were among the most frequent first victims of the outbreak.
Additionally, doctors in these relatively populous countries are extremely few, so people rely much more on family or traditional healers for care. This, too, led to Ebola’s spread, because such intimate contact with dying victims is necessary to contract the disease. Ebola is also transmitted by contact with dead bodies, so burial rites that include ritual cleansing by family members also facilitated its spread.
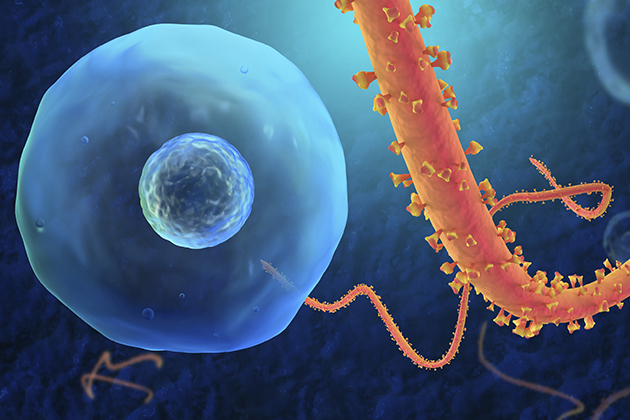
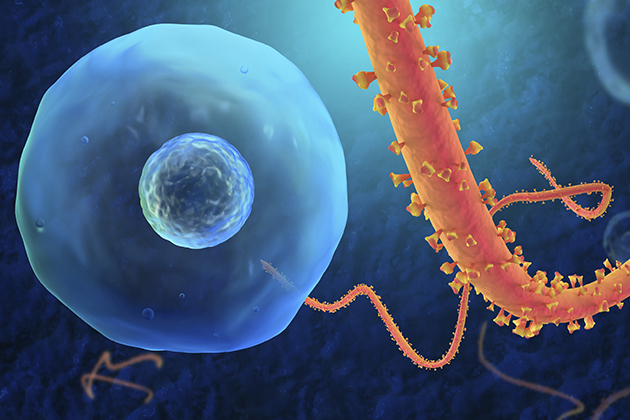
Ebola is a viral disease that is not transmitted like the flu. Flu viruses infect the lungs of ill people, while Ebola infects tissues that line the intestines and blood vessels that underlie the skin.
Flu spreads when flu viruses leave lung cells and enter fluids in the respiratory tract, and can be expelled through coughs and sneezes. Those infectious particles can then be inhaled or swallowed and so transmit the flu to others.
Since Ebola viruses do not enter lung tissues, they cannot be transmitted through sneezing and coughing, but instead enter fluids that exit the body out of the intestines or, less so, through the skin, in sweat. Unlike the flu, Ebola cannot be transmitted before symptoms appear. When victims reach the stage when the virus is shedding through bodily fluids, they are typically too ill to travel. Mr. Sawyer apparently hid his symptoms, and airline personnel were not looking for ill travelers at that time. Air travelers in the affected region are now monitored for symptoms, and screenings are in place elsewhere as well.
Ebola is unlikely to spread to the U.S. Travel restrictions to the most highly affected countries are in place and are likely to increase until the rate of infection moderates. Screening of travelers in airports in West Africa and inspection of passengers arriving from that area are in place around the world. Currently, the U.S. Centers for Disease Control (CDC) have warned U.S. passengers not to undertake nonessential travel to Guinea, Liberia, and Sierra Leone.
Even if a traveler from West Africa were to come to the U.S. and then fall ill, Americans typically do not rely on family members for treatment, but instead go to a doctor or hospital. There the disease will more likely be recognized, and the patient placed in isolation to prevent its spread. Even if a person were to die alone at home, medical personnel with training to enact strict quarantine procedures would be called in to prevent exposure to the victim, and so stem the spread of the virus.
Although the early symptoms of Ebola are not remarkable, they rapidly become worse, lessening the chance that an infectious person can transmit the disease in public. Early symptoms of Ebola include fever, headache, aches, and weakness. Vomiting and diarrhea can set in early, too. Symptoms arise up to 21 days after exposure, but typically develop in eight to 10 days. Bleeding, the symptom most known for the disease and the one most exploited in movies, occurs later and can be both internal and external.
Ebola is highly virulent, but not very contagious. Virulence means the ability to cause infectious disease and the severity of that disease. One measure of virulence is the number of virus particles needed to cause an infection, and for Ebola that is 1-10 viruses, according to the Health Agency of Canada.
A more useful measure is contagiousness, which takes into account how a disease is transmitted and the effect of contact with an infected person. Doctors can estimate the average number of people likely to catch the illness from a single infected person by calculating a number called the reproductive rate for a disease agent. This number can vary in different countries, because infection control measures and the extent of vaccination in a population are also factors in this calculation. The reproductive rate includes the number of contacts an infectious person makes, how long a person is infective, and the likelihood that an infected person will transmit the infection. In the U.S., the reproductive rate for Ebola has been estimated to be 1-4. Measles, by comparison, has a reproductive rate of 12-18; mumps, 4-7; and polio, 5-7.