UConn Health is beginning to recruit patients for the world’s first personalized genomics-driven ovarian cancer vaccine clinical trial. The goal: to prevent an often deadly relapse of the disease in women diagnosed at advanced stages.
The pioneering injectable vaccine OncoImmunome works by boosting the patient’s immune response to enable it to destroy ovarian cancer cells should they resurface. The FDA approved the human clinical trial testing of the experimental vaccine therapy following published research findings showing its effectiveness in reducing cancer growth in animal models.

The new clinical trial will begin with the enrollment of 15 women with stage III or IV ovarian cancer at initial diagnosis or first relapse who will be closely followed for two years – the timeframe with the highest risk of disease recurrence.
Clinical trial candidates include women diagnosed with advanced stage III or IV ovarian cancer who will have traditional surgery at UConn Health where tumor samples will be collected and can be utilized for vaccine production, followed by standard chemotherapy. If cancer-free after traditional treatment, the women will each receive their personalized vaccine injections once a month for six months. Also, each month their blood will be drawn and evaluated for immune response.
The clinical trial will be led by Dr. Susan Tannenbaum, chief of the Division of Hematology & Oncology at the Carole and Ray Neag Comprehensive Cancer Center at UConn Health. Co-investigators are Dr. Molly Brewer, chair of the Department of Obstetrics and Gynecology and Karen Metersky, APRN.
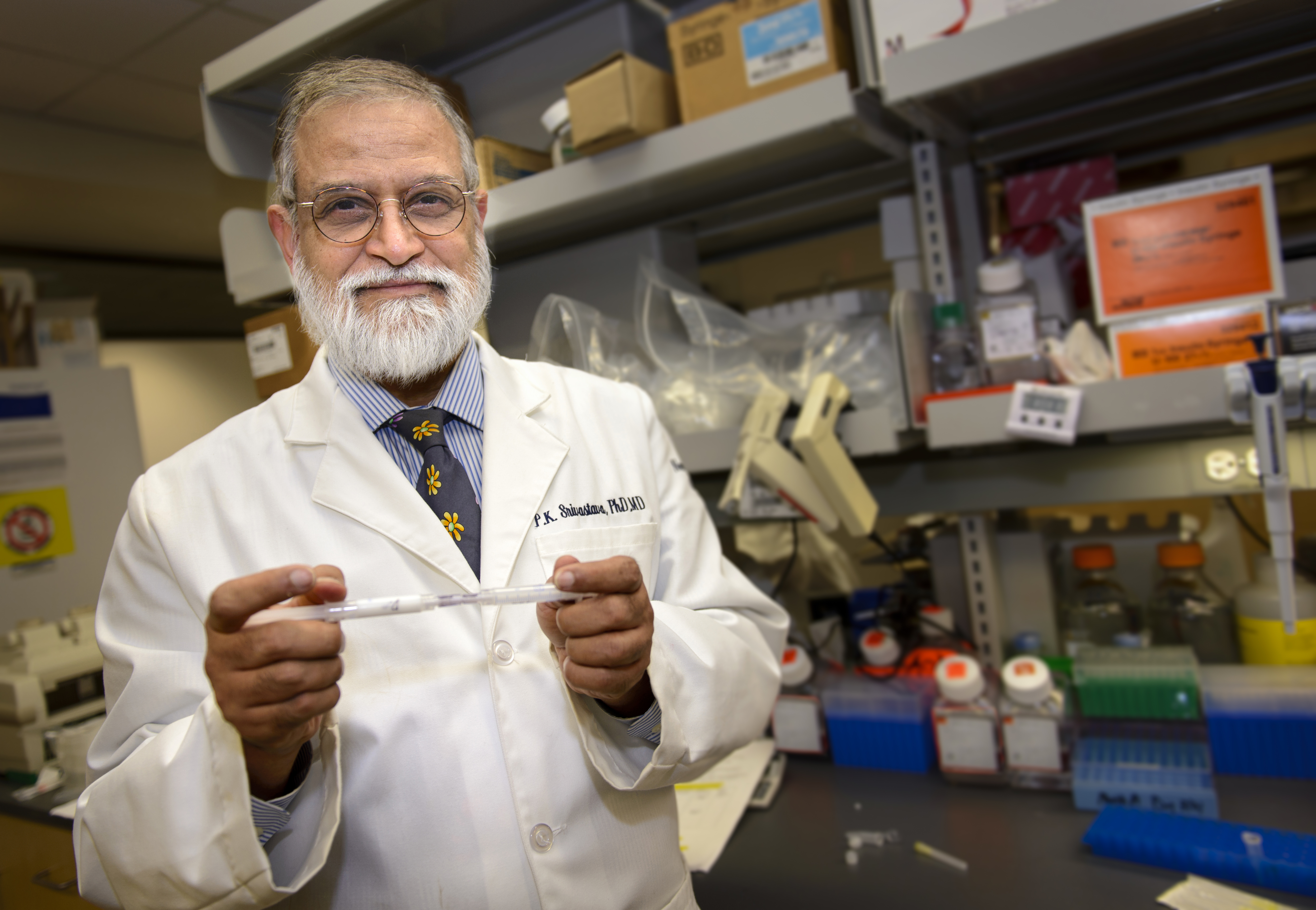
“We are pleased that this moment has come,” says the vaccine’s inventor and immunotherapy expert, Dr. Pramod K. Srivastava, director of the Neag Comprehensive Cancer Center at UConn Health. “This clinical trial will test the power of a patient’s own immune system to prevent recurrence of this often fatal disease. We hope this vaccine can fill the huge gap in therapy options for ovarian cancer patients and potentially bring a long-term solution and cure for women battling the disease.”
Srivastava adds: “Since this trial is a first of its kind, there are a lot of unknowns. We are hopeful the study will answer some of them.”

Each vaccine is individualized for each woman and created using samples of her own DNA from both her unhealthy cancer cells and her healthy blood cells. Over a period of about two weeks, scientists sequence and cross-reference the entire DNA from both sources to pinpoint the most important genetic differences. These genetic differences constitute the ID card, or fingerprint, of that particular patient’s cancer, which is unlike the ID card or fingerprint of any other person’s cancer. Based on the cancer’s fingerprint, bioinformatic scientists led by Ion Mandoiu, PhD, of the School of Computer Sciences and Engineering at UConn in Storrs design the personalized vaccine to target the patient’s cancerous cells specific genetic mutations.
According to Srivastava, this immunotherapy trial has the potential to lay the foundation for similar genomic-driven personalized cancer vaccines against other major cancers such as prostate, bladder, stomach, colon, breast, lung and other cancers.
This year, the American Cancer Society estimates that about 22,440 women will be diagnosed with ovarian cancer and approximately 14,080 women will die from the disease. Why? Currently, there is no early-screening test for ovarian cancer and no effective long-term treatment. It is often diagnosed at advanced stages following the surfacing of non-specific abdominal symptoms such as bloating. But even after a woman is successfully treated with traditional surgery and chemotherapy, the disease has a very high chance of coming back. Tragically, most women die within five years of their diagnosis.
To learn more about the new clinical trial and its enrollment, please visit: here.