Twenty eight-year-old Ashley Derungs-West and her husband, Austin, planned for a peaceful home birth for their first child, but at 24 weeks her pregnancy took a sudden and unexpected turn. Pre-eclampsia, which is a common concern during pregnancy, was her initial fear for keeping them from a home birth, yet she was in disbelief when her medical emergency was diagnosed as a stroke from a heart defect.
Derungs-West woke up in the middle of the night unable to feel the right side of her body and attributed the numbness to sleeping in an awkward position. When the sensation returned along with a headache, she associated the symptoms with her usual migraines. She was exhausted when she woke in the morning, so napped all day.
When she returned to work the following day, she had a headache and struggled to read the computer screen. She reached out to her midwife who suggested she go to the hospital to be assessed. She drove herself to UConn John Dempsey Hospital and was admitted to labor and delivery.
A rapid response was initiated to evaluate a potential stroke. A series of tests were conducted including a CT scan and an MRI.
The baby was on a monitor, and Derungs-West was relieved to learn that she was okay. As all the tests were being performed, she kept thinking she was overreacting, and this was caused by stress.
Late that night, Maternal-Fetal Medicine (MFM) subspecialist Dr. Corinne M. Weeks, Cardiologist Dr. John Glenn Tiu and Neurologist Dr. Priya Narwal informed her that she had suffered a stroke.
“I thought they were crazy; I didn’t have a stroke, I have a friend who had a stroke, and he was in a wheelchair,” she says. “It was not what I imagined having a stroke was like. I was in denial.”
Stroke and Pregnancy
The overall incidence of stroke in pregnant women is three times the amount compared to non-pregnant reproductive age females with the incidence of 30 per 100,000 deliveries. Stroke can occur at any time in pregnancy but most commonly in the first two weeks postpartum.
Unfortunately, strokes can sometimes present with symptoms that are easy to overlook or attribute to other conditions, especially during pregnancy when many changes occur in the body. It’s fortunate Derungs-West sought medical attention when she did, since timely intervention is crucial for the health of both mother and baby.
MFM subspecialist, and MFM fellowship program director, Dr. Andrea Shields explains that during pregnancy a woman experiences a hypercoagulable state, when the blood clots more as a natural way to lessen blood loss during labor and delivery. Preeclampsia and gestational diabetes can also increase the risk for blood clots to develop during pregnancy.
Shields developed the Obstetric Life Support (OBLS) Guidelines for stroke in pregnancy and UConn Health’s Labor and Delivery department is the first and only in the country to use the guidelines.
Derungs-West was admitted to the Intensive Care Unit (ICU) where she spent four days. The numbness and blurry vision kept returning.
“The numbness was scary and would last a few minutes to an hour,” says Derungs-West. “Every time I tried to stand my leg would go numb and I could not walk.”
The baby monitor continued to reassure her that the baby was okay.
It was concluded that she had a cryptogenic stroke, which does not have an identifiable cause and accounts for one-third of all strokes. After ruling out other causes, it was determined there was a presumptive patent foramen ovale (PFO), a hole between the left and right atria (upper chambers) of the heart. This hole exists in everyone before birth, but most often closes shortly after being born.
“To be able to prevent recurrent stroke, it is extremely important to first identify the cause of the stroke and address it. Which is why it was so important for Ashley to undergo the extensive testing that she did while being admitted to the hospital, which helped us to identify the heart defect and address it appropriate,” says Narwal. “Strokes, while rare in pregnancy, can have a significant impact on the patient’s quality of life hence it is important to be vigilant and seek immediate medical attention in the event of new neurological symptoms.”
The case required the collaborative effort of the multidisciplinary team of specialists that including members of the cardiology team Dr. Tui, Dr. Supriya Tigadi, and Dr. Juyong Lee; along with Dr. Narwal in Neurology; Dr. Shields in MFM; and Dr. West in OB/GYN to manage the complexities with the goal of preventing another stroke and delivering a healthy baby.
“It was so reassuring to have a great team at UConn,” says Derungs-West. “Neurology, Cardiology, and MFM were all super great and would meet regularly and provide me updates.”

The team determined it was best to manage the prevention of another stroke and focus on the heart defect after the delivery of the baby. Derungs-West was started on a blood thinner and aspirin and took it until the heart surgery.
“I had to give daily injections for the blood thinner and was covered in bumps and bruises; dealing with being pregnant and then all this on top of it was hard,” says Derungs-West. “Dr. Shields was the best communicator and helped me get through it all. She was so kind.”
On May 13, Derungs-West was induced and a healthy baby girl, Lorelai, was born.
She spent the following week in the hospital to control the risk of stroke and had cardiology procedures that were a risk to do during the pregnancy to confirm the PFO.
The Heart Defect
Interventional cardiologist Dr. Juyong Lee, director of the structural heart program at the Pat and Jim Calhoun Cardiology Center at UConn Health, explains that the opening in the heart is necessary to maintain life in the womb by breathing through the mother’s blood that enters the baby through the opening in the heart. Once born, the flap will close for most; however, for 25-30% of population, it stays open. The flap is not fused so opens and close if anything floating inside such as a clot, it can cross to the left atria, and go to the brain, causing a stroke.
He explains that the pregnancy may have predisposed Derungs-West to a compressed vein in her pelvis that could lead to a clot because the blood flow becomes more sluggish. When the presumed clot dislodged from the left leg vein, it traveled through the venous circulation and entered through the left side atrium and crossed through the hole to the left side without going to the lungs and went to the brain leading to a presumptive stroke.
It was decided to close the hole as studies show that younger people have a 69% reduction in risk of recurrent stroke when closing the hole versus medical therapy alone.
On June 10, Lee performed the percutaneous PFO closure. During the procedure the patient was given a local anesthetic, and a small incision was made in the groin, a catheter inserted into a blood vessel and guided to the heart. After positioning a closure device on each side of the PFO, the device was released to remain permanently in the heart.
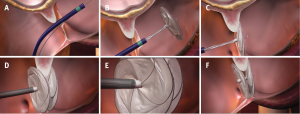
The outpatient procedure typically takes one to two hours. After the procedure, the patient’s body tissue will grow over and around the device, and within three to six months, the device will be completely covered by heart tissue and become part of the heart wall.
Most of the population who have a PFO are fine and are unaware, like Derungs-West, unless there is an issue like stroke.
“This case was unique, regarding the young age of the patient having a stroke during pregnancy, and successful management with the multidisciplinary care among OBGYN, MFM, Neurology, and Cardiology at UConn Health was key to a successful outcome,” says Lee.
“Dr. Lee was amazing and made me so comfortable about the heart surgery that he performed to close the hole.” Says Derungs-West.
Ashley and Baby Now
While the pregnancy did not turn out the way that Derungs-West and her husband had planned, she feels grateful that the clot landed where it did, and she and the Lorelai are healthy.
After the heart surgery she had some chest pain when lifting the baby, but Lee performed an ultrasound, and all is okay.
“It was so overwhelming being a new mom and feeling like I had no control over what my body was doing,” says Derungs-West. “It was very scary for Austin watching me go through all this as well.”
Derungs-West has minimal lingering side effects from the stroke – she sometimes gets headaches on the left side, where the stroke was. Now that the hole in her heart is closed, she does not fear another stroke.
She follows up with Dr. Narwal in Neurology and Dr. Tigadi in Cardiology, takes aspirin every day, and is back to work.
“I am so grateful for everyone at UConn Health. Everyone there was so amazing,” says Derungs-West.



