When it comes to caring for sickle cell disease patients UConn Health is leading the way forward.
Leading the charge is Dr. Biree Andemariam, director of the New England Sickle Cell Institute at UConn Health, the first and only dedicated center of its kind in the region.
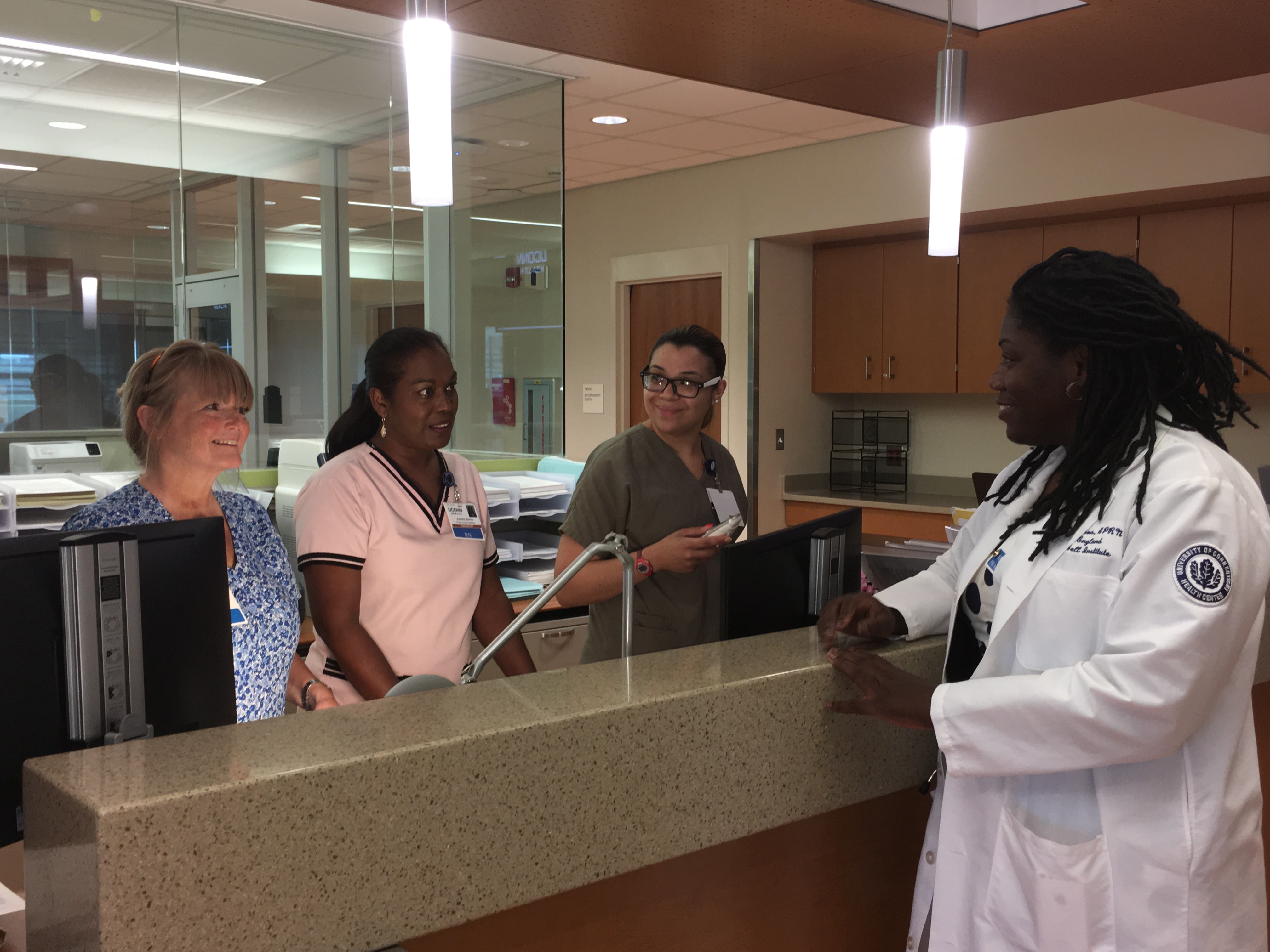
This August, UConn Health opened a new outpatient center for sickle cell patients. The brand new facility is conveniently located on the fourth floor of the new, state-of-the-art hospital tower at UConn John Dempsey Hospital. The center allows for both scheduled outpatient comprehensive care visits as well as same-day urgent care for management of sickle cell disease exacerbations such as severe pain, dehydration and worsening anemia.

The sickle cell center has a large patient care area with ten private acute care suites, five exam rooms, and two specialized blood transfusion rooms. Also, conveniently located in the same building is the Emergency Department and the hematology inpatient care unit for any critical care patient needs.
The new unit is a dream come true for Andemariam. When she arrived to UConn Health in 2007 she noticed a recurring patient care pattern. Sickle cell patients would come to the Emergency Department with repeated episodes of severe pain and experience prolonged hospital stays.
“I knew I could do something about this,” says Andemariam.
In 2009, she established at UConn Health the first longitudinal clinical program in the region to help adults combat the daily suffering associated with sickle cell disease and improve their overall quality of life. She also worked to identify more sickle cell patients in the surrounding communities to help them better manage their health, reduce their pain symptoms and disease complication risks, and to keep them out of the hospital so they could enjoy their lives more.
Since the establishment of the program, several new care services have been developed, including a pediatric sickle cell patient transition program with Connecticut Children’s Medical Center, the first program in the state for advanced whole blood transfusions via automated erythrocytapheresis and personalized pain management algorithms for acute care visits.
The small program has now grown from just a dozen patients to now comprehensively serve more than 220 patients living with sickle cell disease.
“Last year, our New England Sickle Cell Institute surpassed their goal of reducing hospitalizations and visits to the Emergency Department, while increasing patient visits to our day clinic,” said Wanita Thorpe, administrative manager of the Carole and Ray Neag Comprehensive Cancer Center at UConn Health which the Institute is a part of. “Now outpatient sickle cell services moving into the same building as the ED and hematology inpatient care will allow Dr. Andemariam and her team to better manage the health of these patients.”
Increasing Awareness of Sickle Cell Disease
Sickle cell is a devastating and painful inherited red blood cell disease. Sadly, life expectancy for the majority of people with sickle cell is age 40 or less.
An individual born with sickle cell has red blood cells that are abnormally hook shaped which affects the blood’s circulation in the body. The name of the disease was first coined by its discovering physician after the cells under his microscope he thought resembled a sickle, a traditional farmer’s tool used for crops. The first case of sickle cell was initially described in the western medical literature in 1910. But even more than 100 years later there are no real therapies to treat, fully prevent, or reverse its pain.
Millions are affected worldwide by sickle cell disease including 100,000 Americans. Globally it tends to affect those of African, Mediterranean and Indian descent. In the United States, African-Americans and Latinos are predominantly affected.
“Sickle cell is a rare, orphan disease affecting underrepresented minority communities in our country, and there needs to be more research dollars dedicated to finding new therapies and a universal cure, along with more advocacy for this fragile and suffering patient population,” stresses Andemariam.
The inherited disease is typically first diagnosed at birth through state-mandated newborn screening. Individuals with sickle cell have profound anemia, which means they don’t have a healthy level of oxygen-rich red blood cells circulating in their body. In fact, their blood level is usually nearly half that of a healthy individual. A significant number of patients are destined to a lifetime of monthly blood transfusions to minimize common complications including pain and risk of stroke.
The most common symptom patients experience is severe pain due to the development of blockages in their smaller blood vessels and capillaries when their abnormally shaped red blood cells cannot pass through smoothly and get stuck. In addition to causing severe pain, these blockages can also lead to stroke and compromise the health of vital organs such as the kidneys, lungs, and the spleen. The blockages can reduce blood flow and cause blood infections such as sepsis leading to death.
“Basically, sickle cell causes a patient to experience blockages around the body that are like having excruciatingly painful, mini-heart attacks constantly,” says Andemariam.
To manage the condition Andemariam and her team treat patients with very strong pain medication and in some cases monthly blood transfusions. However, since there is not great awareness of the disease and no way to immediately test for it sickle cell patients may not be appropriately or rapidly cared for when they go to their local urgent care or Emergency Department. Depending on the clinical setting’s resources, the blood test to confirm the disease tends to take hours to a few days.
In light of this, individuals with sickle cell often are met with bias and stigma when they go to local acute care centers with pain and ask for the narcotics they need to treat it. This is exactly why a dedicated home for this population of sufferers is needed and why UConn Health’s new center proves the commitment and dedication UConn Health’s senior leadership has entrusted to Andemariam and her team to provide an exceptional space for this population. “We wouldn’t have been able to grow this center without their support and the tireless dedication of the nurse practitioners, nurses, social workers and medical assistants who care for our patients with the highest level of commitment every single day,” says Andemariam. Her team’s comprehensive care approach ensures that each individual patient’s acute care needs are met including any for social work and psychotherapy needs.
However, to help circumnavigate the challenges sickle cell patients may face in an emergency care situation, UConn Health has partnered with the Red Cross to develop a new identification card program to speed patient care.
“Sickle cell is a terrible and debilitating disease, with individuals struggling to live a normal life despite their frequent severe pain episodes and other serious complications,” says Andemariam. “Patients live every day knowing they are not expected to live long. Often, their foreshortened life is filled with pain, suffering and the lack of available treatment options.”
Currently there are about 1,000 adults in the state of Connecticut affected by the disease and Andemariam is on the hunt to help more. She does continuous community outreach at civic and church organizations to identify more adults with sickle cell with the help of the local chapter of the Sickle Cell Disease Association of America. In addition, UConn Health has formed a collaboration with Connecticut Children’s Medical Center to formalize a process to seamlessly transition their 200 sickle cell pediatric patients they care for to UConn Health as they reach adulthood.
“My hope is to ensure that those living with sickle cell don’t spend the majority of their lives in pain or in the hospital, and get the regular treatments they need without delay to limit their risk of pain, stroke and other complications at every chance possible,” says Andemariam. “We are committed to bringing increased awareness of this disease while tirelessly conducting research to answer key questions.”
The New England Sickle Cell Institute has partnered with the Buffalo Soldiers Motorcycle Club of Hartford to help raise awareness and funding to further support sickle cell research initiatives at UConn Health. On August 13th, the club will host their 2nd annual sickle cell ride for research. This partnership serves as a means to educate communities about the disease and how to better support its patients.
To learn more about UConn Health’s New England Sickle Cell Institute visit, here.